IN FOCUS: The challenges young people face in seeking mental health help
Suicide continues to be the leading cause of death for youths, with a total of 71 people aged 20 to 29 taking their own lives last year. CNA looks into why some young people delay seeking mental health treatment, despite growing awareness in Singapore.

Young people in Singapore face several challenges when seeking help for their mental health. (Graphic: Rafa Estrada)
SINGAPORE: Kevin* has known his mind “works differently” ever since he was in Secondary 3. Things like grocery shopping may be therapeutic for some, but it is an incredibly stressful task for him.
“It’s always the difficulty of choice in making the simplest decisions, like what kind of pasta should I buy? I can take 15 minutes just standing there before deciding which to buy,” he said.
Kevin did not know then that he had anxiety, which can interfere with decision-making. What he was familiar with, though, was the common refrain that he would hear from people around him urging him to stop worrying and thinking too much.
He went on with life struggling with not feeling “fully normal”. It was another 13 years before he stepped into his first therapy session.
“It took me quite a while to say that I wanted to seek help,” said Kevin, who is now 29 years old.
“People always think that it’s (mental illness) just a phase, until it becomes too serious...I don’t want to eventually (commit suicide).”
Statistics from the Samaritans of Singapore (SOS) last week showed that the number of suicides in Singapore for those aged in their 20s remained the highest last year compared to those in other age groups.
A total of 71 people aged between 20 and 29 killed themselves in 2019. Suicide continued to be the leading cause of death for those aged 10 to 29 last year.
READ: Number of suicides among those in their 20s highest in Singapore
While Kevin took the first step to seek help after a long struggle, not everyone does so.
According to a Singapore Mental Health Study conducted in 2016, while one in seven in Singapore has experienced a mental disorder in their lifetime, more than three-quarters did not seek any professional help.
Respondents cited a “treatment gap” of 11 years as the median time between when they first experienced symptoms and when they sought help for obsessive compulsive disorder.
It was four years for bipolar disorder and alcohol abuse, two years for generalised anxiety disorder and one year for major depressive disorder.
READ: 60,000 subsidised outpatients seek treatment for mental disorders each year: Gan Kim Yong
In the same study, youths between 18 to 34 years were presented as the most vulnerable group - one in five would have experienced a mental disorder in their lifetime.
In Singapore, there is a comprehensive network of mental health services - from helplines and Voluntary Welfare Organisations (VWOs) offering youth-centric counselling services, to clinics at government hospitals and in private practice.
However, some young people experience challenges in seeking professional help.
NAVIGATING MENTAL HEALTH SERVICES
Mental health awareness among young people appears to be growing.
According to the Ministry of Health (MOH), from 2017 to 2019, an average of 12,600 patients aged 15 to 34 years sought treatment for mental health conditions at public hospitals each year.
The Community Health Assessment Team (CHAT) - a community-based youth mental health outreach and assessment initiative - received around 1,800 referrals and conducted assessments for about 770 youths last year.
That is 36 times more referrals and 15 times more assessments than 2009, when the initiative was first launched.

In March, then Senior Minister of State for Health Dr Lam Pin Min said during the Committee of Supply debate in Parliament that recent engagements with young people showed "mental well-being continues to be a top concern".
In response, a new initiative offering mental health support and awareness to at-risk youths is expected to launch in the second half of 2020.
The Integrated Youth Service, jointly developed by the MOH, Institute of Mental Health, Agency for Integrated Care and Care Corner, was described in an MOH press release as a "one-stop service where at-risk youths can access coordinated mental health and support services such as individualised basic emotional support, needs identification and befriending services".
Responding to queries from CNA, MOH said that the Integrated Youth Service began community outreach in the “Northern region in April 2020”.
“In the midst of COVID-19, Care Corner’s mental health department, INSIGHT, has had to adapt its outreach to youths through alternative online platforms such as Instagram, a Telegram bot and webinars,” it added.
To date, these platforms have reached out to over 500 users.
READ: Mental health support service for at-risk youths to be launched this year: MOH
This resource may be a welcome addition to helping young people navigate their way through the range of options so they can find a solution that works.
Broadly, there are two approaches for treating mental health conditions: Medication and psychotherapy - both of which can be used on its own without another, with different effects on an individual.
“Medication reacts differently for different individuals even if it’s the same condition - a certain medication may work perfectly well for one, but for another it can have more complicated side effects,” said Mr Jackie Tay, the executive director of PSALT Care, a registered charity and mental health recovery centre.
On the other hand, psychotherapy and counseling involve the “human factor” or the social connection between the clinician and the patient.
“It’s the chemistry and connection - some patients would connect better with certain styles of therapists. You also need to navigate around that,” said Mr Tay.
As such, the continuum of care for mental health conditions can also be long, intensive and complicated. For example, one young adult whom CNA spoke to likened the process of finding suitable treatment to finding a soulmate on matchmaking sites like Tinder. Kevin agreed.
Finding suitable treatment requires time and effort from an individual. However, experts CNA spoke to suggested that improving the quantity and quality of information about mental health resources may encourage a young person to take the first step to seek help.
“This group of vulnerable people (with mental health issues) would already be cognitively overloaded,” said Ms Anthea Ong, a former Nominated Member of Parliament who advocated for the prioritisation of mental health in the budget 2020 debate.
She added that while the National Council of Social Service provides a list of available mental health resources online, there should be a “community navigator” that goes beyond “just information”.
“There's no guidance on where to go, the cost fees - at least list down some of the possible journeys or experiences and then map that.
“It’s not a site that helps you to navigate the services available,” she explained.
For those like Aisha*, who engages in self-harm and suspects she has depression, the plethora of options that a Google search presents her has posed a hindrance.
“I remember Googling ‘Singapore counselling session’ and ‘affordable counselling’... but there isn’t a site that narrows down your options for you or tells you what kind of treatment is appropriate,” the 23-year-old patient service associate at a local hospital said. She has yet to see a professional.

As much as there are many avenues of care out there, there may not be enough education on selecting an appropriate one, said Dr Tracie Lazaroo, a clinical psychologist from Inner Light Psychological Services and LP Clinic.
“Finding the appropriate mental health service can seem like an overwhelming experience.”
Kevin for example, did not know the difference between a psychiatrist, a medical doctor who can diagnose mental disorders and prescribe medication, and a psychologist - someone who specialises in modes of therapy.
While he was hoping to speak to a therapist about his problems, he unknowingly set an appointment with a psychiatrist at a private hospital instead, who prescribed him medication like Lexapro and Xanax.
“I didn't know where to start and where to search … (the private hospital) came out with the first few searches of Google,” he said.
“I was quite taken aback because it was more of a clinical setting (with the psychiatrist) and it was not very nice. I didn’t feel very comfortable.”
Mr Tay added that the awareness of the availability of health and resources has not increased significantly over the last five years, neither has the “ease of search”.
“For example, we know that when there’s a fire, we call 995. When you need the police, you call 999. But when you've got a mental health problem, who do you call?”
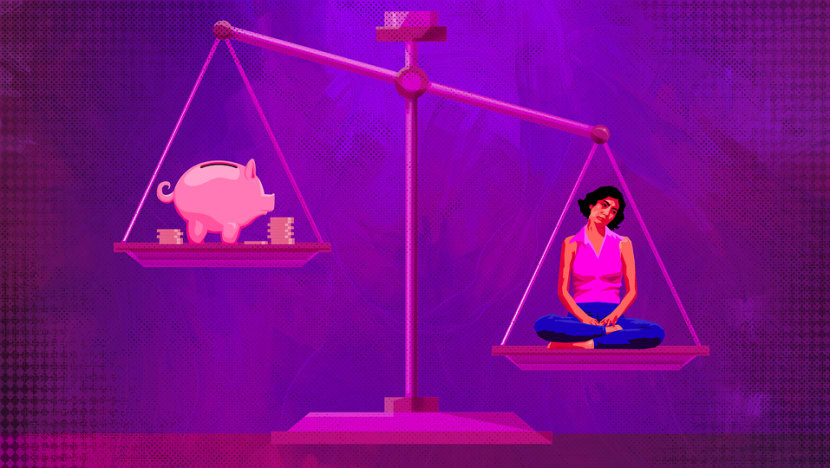
THE PRICE OF MENTAL HEALTH TREATMENT
Given the long-term nature of mental health treatment and recovery, financial concerns can be a factor in deciding whether to seek help, experts said. Most youths who spoke to CNA also said that the cost of treatment has been a concern.
Under the Chronic Disease Management Programme (CDMP), patients with schizophrenia, major depression, bipolar disorder and anxiety can withdraw up to S$500 from MediSave per year to defray the cost of outpatient treatments such as therapy and counselling treatment.
Each claim is subjected to a 15 per cent co-payment in cash.
To receive further subsidies at the Institute of Mental Health (IMH) - Singapore’s only tertiary psychiatric care institution - one can get a referral from a doctor at the polyclinic. The first consultation costs S$40 and S$37 for the subsequent ones.
This is much cheaper compared to private clinics that charge anything between S$100 to S$250 for one session - depending on the training, specialisation and experience of the clinician.
For example, Raffles Medical Group states on its website that a session with a counsellor or psychiatrist will cost at least S$160.50 and S$214 respectively.
While there are government subsidies available at public healthcare institutions, Dr Lazaroo said that some patients need prolonged care.
“These disorders require consistent long-term care on a weekly basis especially within the first year of symptom onset, commonly spanning over the course of a few years,” she added.
“Unfortunately, some of these patients may struggle maintaining employment while receiving therapy or psychiatric treatment, which will inevitably cause them to have insufficient MediSave or MediShield Life funds.”
The cost of weekly treatment will also “stack up very quickly”.
To further encourage help-seeking behaviour, Ms Ong said that there is a need to “do even more” to keep mental healthcare affordable in Singapore because mental illness “does not necessarily have any obvious physical symptoms” and treatment will not take “just one session”.
She noted the difference in inpatient MediSave claims - while the daily limit is S$450 for physical illnesses, it is S$150 for psychiatric treatment.
“The claims limit is already lower compared to physical health conditions and you might need to go for more treatment. It’s a double whammy,” Ms Ong added.
During the Ministry of Health’s 2020 Budget debate in Parliament, then-Minister of State for Health Dr Amy Khor said that MOH reviews the amount of financial support regularly to ensure that it is adequate.
Based on the latest data, fewer than three in 10 persons’ subsidised bills exceed MediSave’s daily withdrawal limit, she said.
However, financing for treatment may be a challenge for those with conditions not covered by CDMP such as post-traumatic stress disorder and eating disorders, according to the experts CNA spoke to.
In an email response to CNA’s queries, MOH said that from Jan 2021, patients with “complex chronic conditions” will be eligible for a higher annual MediSave withdrawal limit of S$700.
“No one will be denied appropriate healthcare because they cannot afford to pay. Those who cannot afford their treatment at the public healthcare institutions even after subsidies, MediShield Life and MediSave, can approach the medical social workers for MediFund and other financial assistance.”
Even so, experts highlighted that treatment at a private clinic or voluntary welfare organisation (VWO) may be more suitable for some but that means they would have no access to MediSave withdrawals.
“If you are seeing a psychologist every week and you can’t afford it because the fees are not claimable, you will have to stretch your therapy. Consequently, it takes that much longer to get well,” said Mr Tay.
That is something that Ms Aleesha Khan can relate to. The 23-year-old was diagnosed with generalised anxiety disorder, depression and PTSD nine years ago and sought treatment at IMH’s Child Guidance Clinic for about five years.

Ms Khan went on to seek treatment for PTSD at a private clinic, where she received Eye Movement Desensitisation and Reprocessing (EMDR) - a four to six-week psychotherapy treatment that helps to alleviate distress associated with trauma.
As useful as that may be, she is paying about S$235 for every session.
“It’s worth it because it’s helping me, but it’s so much money. Not everyone can afford that and there’s no way to get subsidies because they just don’t cover it,” she added.
On top of that, she is also seeing a therapist to help with her anxiety and depression. To save money, she makes the “conscious choice” of going for one monthly session, if not it would “really be too much”.
“If I had a choice, I should actually be going to therapy more often...(but) I’m already spending S$235 a month, at least S$2.8k a year just on therapy,” Ms Khan said.
“I’m middle-class but I know so many people who need it but they can’t afford it."
SELF AND SOCIAL STIGMA STILL EXIST
“It’s like waves and waves of sadness...you feel like the world is not a place for you.” This is how being depressed feels like to Aisha, who said she maintains a “strong look” daily even though she can break down several times in private.
“It’s especially hard to be working in healthcare because you can’t show that to your colleagues or patients. But at the end of the day, when you go home and you are left alone to your thoughts - that’s when it really kills me,” the patient service associate said.
While Aisha has been considering seeking help ever since she was in secondary school, the idea of receiving a diagnosis and “being sick” scares her.
“It’s like, ‘I’m working in the medical line and I’m like that?’ I think that will be the perception of people ... so I just suck it up,” she said.

The perpetuation of stigma can come from various sources, such as the public, family or even within oneself. Young people are also more prone to its effects as they are in a “developmental phase” where they are trying to “form their identity”.
“They might be self-conscious and are typically more concerned about how others may see and perceive them, especially so by like-minded peers,” SOS added.
“To avoid being judged or associated with the perceived negative stereotypes, youths may choose to hide their struggles in order to avoid being seen as ‘weak’ ...even if they harbour thoughts of suicide.”
“There’s probably a very big mindset difference,” said Ms Charlotte Chen, a therapist from Counselling & Care Centre.
“I noticed that (youths) seem to be more open to sharing with their peers than adults, especially their parents. They have the impression that their parents won’t believe that mental illness is real.”
Most youths that CNA spoke to have not told their families about seeking treatment or their struggle with mental health.
*Kiara, a 27-year-old early intervention teacher said it took her a few years before she went to a professional for her depression and borderline personality disorder as she came from a “very religious, conservative family”.
“Anytime they see me feeling sad, or angry, their first advice to me is to seek God. They mean well but these words are not really effective… (they don’t understand that) it's the brain chemicals in your brain that's going off,” she said.
“So I just kept telling myself, it's okay I can handle this. What's the point of seeking help when I'm gonna end up dead anyway?”
Similarly, 27-year-old Yi Wei* said that it is “very disheartening” whenever she brings up the topic of mental health with her parents.
“They don’t understand what it is … they just see it as something difficult that you have to overcome like everything else in life.”
The account executive added that while “working very hard” is one of her outlets for coping with depression, doing well in school or at work has not helped in convincing her parents that mental health treatment is necessary.
“That translated to my parents thinking, ‘She's doing very well in school, so it’s not as bad as what she makes it out to be? How can it be so hard when you are actually excelling?’”
“Living with that sort of mentality within your family is hard. That’s why it took me so long to get diagnosed and seek help,” she added.
Not only is “destigmatising” mental illness important, there is also a need to undo the “narrative” that it only happens to certain individuals, said Ms Anthea Ong.
“Kids might think, ‘My parents send me to a good school, I’m from a well-to-do family and all that - how can I have this issue? I have everything I want.’ That’s when they start to beat themselves up, thinking they are self-indulgent.”
She added: “But that is not true ... there are so many ways to be challenged mentally in the society that we’re living in.”
THE ONES WHO FILL THE GAP
While affordability and uncertainty about who to turn to are key barriers for some young people who need mental health treatment, there are charities and VWOs aiming to address some of those concerns.
Shan You Counselling Centre, for example, charges S$80 for every hour of counselling and offers a 50 per cent subsidy for students.
“In some instances, some of the young people may still not be able to afford (it), then we will offer further subsidy,” said its director Dr Kum Yew Siew.

Dr Kum added that seeking help at VWOs or private clinics does not require a referral unlike in public hospitals where a psychiatrist will have to make a diagnosis before someone can be directed to a psychologist.
“Not only is there a delay but also on a psychological level, having to go through multiple professionals and having to decide whether you even want to go through multiple people before you can talk to someone can pose as a barrier.”
“In my opinion, you do not need a diagnosis to provide help and intervention,” he said.
Ms Chen from Counselling & Care Centre added: “When youths come to a counselling centre, we are not trained to diagnose a mental health condition so we work with wherever they are, whatever struggles they're dealing with and we support them from there through talk therapy.”

“Given that we are a VWO, I imagine they feel a little bit safer in terms of their records being kept confidential. That sense of safety and anonymity is really important (to youths),” said Ms Chen.
“Sometimes in seeking employment they might ask if you have any psychiatry issues. If they have received an official diagnosis (at the hospital), I imagine they would face a dilemma of whether they should or should not disclose.”
However, VWOs that CNA spoke to reflected challenges in sustaining affordable services. Ms Chen said that while there was a pro-bono scheme in the past, the centre has not been able to continue that service due to the lack of funding.
“That is a real challenge and struggle. I do have one or two clients who can't quite continue counseling because of the fees,” she added.
The difficulty of fundraising can also be tied to the stigma of mental illness, said Mr Tay from Psalt Care, and this prevents patients from sharing their stories and experiences with the public.
“Most of us in the charity sector ... try to do our best with the limited resources. We would certainly hope we can have more so that we can do more.”
According to MOH’s latest data, NCSS provided S$8.7 million and S$5.7 million in funding to Social Service Agencies (SSAs) for mental health support services and counselling programmes, respectively, in 2018.
While there are counsellors in school and upstream efforts from the Ministry of Education - such as plans to give more focus to mental wellness in the Character and Citizenship Education (CCE) curriculum - Ms Ong suggested that more funding needs to go to “community support” and VWOs.
READ: Schools to offer mental health lessons from 2021; more trips to Asian countries
“It is important to let young people know that there is trusted, third-party support available out of campus that is affordable. We know the ratio of counsellors in school to the number of students,” she added, noting that waitlists exist for university counselling services as well.
“Community mental health agencies can also be a great resource to young people.”
NEED TO “SOLVE STRUCTURAL ISSUES”
As awareness of mental health issues among young people has grown, even more efforts are being put into providing help and support. This includes the 24-hour National Care Hotline launched in April this year, which is manned by more than 300 psychologists, counsellors, social workers, psychiatrists and public officers.
According to MOH, there are consolidated sites that list mental health resources and “function as navigators”, such as the My Mental Health microsite that was launched this year by Temasek Foundation, in collaboration with the AIC.
“It is a resource hub that provides online mental health resources such as mental health-related articles, online forums and information on support groups to support one’s mental health during the COVID-19 period,” it added.
Another website with various resources on mental health was also launched to help users assess their wellbeing and match them with forms of assistance if needed.
READ: COVID-19: One-stop mental health platform launched to match users with resources and helplines
The website, called mindline.sg, consolidates access to many resources and tools to help people "access and navigate care, with an emphasis on stress and coping”.
While there has been a “groundswell” of community efforts in recent years - such as the Beyond the Label campaign by NCSS to address mental health stigma – Ms Ong said that the prevalence of mental health concerns among youths is indicative of the work that still needs to be done.
“That already empirically tells you that as much as we rally on the ground, we are not solving the structural issues of our mental healthcare such as affordability, accessibility and quality.”
READ: AIA launches first insurance policy in Singapore that covers mental illnesses
In the meantime, young people like Ms Khan are playing their part. The psychological science student shares her personal experience in help-seeking and resources on her Instagram page, including a compilation of affordable mental healthcare in Singapore.
“Back then, there weren’t a lot of resources ... a lot of support and answers I needed were not available to me. So my objective (now) is to provide information that I needed as a teenager who was in distress,” she said.
Ms Khan added that she receives many messages from youths who follow her page - some of them needing a listening ear, others looking for information on where to seek help.
“Some get overwhelmed looking at hospital websites...I have my own list that is categorised - if someone comes to me, I make it a point to refer them to the appropriate information,” she added.
“What I really try to do is to make sure that they are as informed as they can be so that they can advocate for themselves.”
*Name has been changed to protect identity
Where to get help: Samaritans of Singapore operates a 24-hour hotline at 1800 221 4444, or you can email pat [at] sos.org.sg. If someone you know is at immediate risk, call 24-hour emergency medical services.














