The Big Read in short: Blood, sweat, tears of Singapore’s frontline heroes against Covid-19

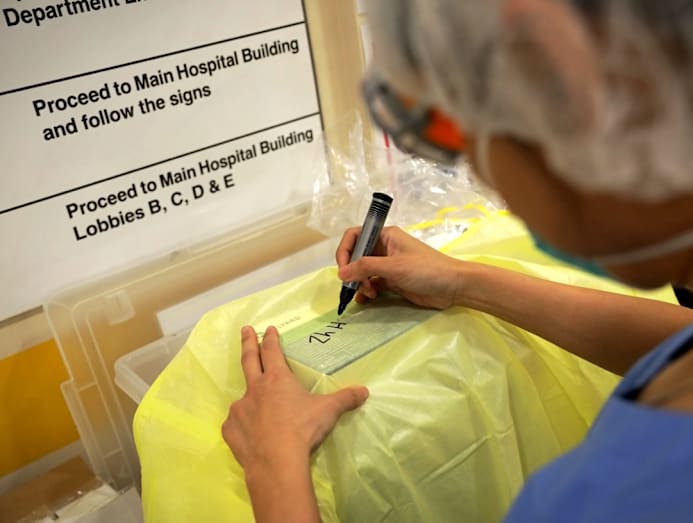
Respiratory and critical care medicine clinicians at the Singapore General Hospital’s Covid-19 isolation ward making sure that the Powered Air Purifying Respirator (PAPR) is donned correctly.
Each week, TODAY’s long-running Big Read series delves into the trends and issues that matter. This week, we look at the personal sacrifices made by healthcare workers at the frontline of Singapore’s fight against Covid-19. This is a shortened version of the full feature, which can be found here.
SINGAPORE — Earlier this month, Dr Chng Woei was asked by her 24-year-old daughter if the family was not going to have dinner with the maternal grandparents until “this dies down”.
“This” refers to the Covid-19 crisis which has hit every continent except Antarctica, and has earlier this week been declared a pandemic by the World Health Organization.
And dinner with the elderly folks was out of the question till the situation improves, the general practitioner (GP) replied to her daughter.
The 51-year-old, who works at Healthmark Medical Clinic in Punggol, would rather be safe than sorry. Since the clinic is a Public Health Preparedness Clinic (PHPC), a network of clinics providing subsidised treatment and medication during public health outbreaks, she could never be certain if the next patient she sees is a Covid-19 carrier, and her worst fear is that she may end up transmitting the virus to her parents who are in their 80s.
That is why she has restricted her family’s visits to her parents’ house to less than 30 minutes each time. Even then, they would not have dinner together, unlike before.
Dr Leong Choon Kit, 53, who runs Mission Medical Clinic in Serangoon, is keeping a distance of at least one metre from his loved ones, including his wife and teenage daughter.
That means sleeping on a foldable mattress at night, while his wife takes the spot on the bed. And there are no hugs and kisses too, he added.
Sacrifices such as these have become part and parcel of life for those working on the frontline in the fight against the highly contagious Covid-19 virus in Singapore, which has seen a total of 200 confirmed cases as of Friday (March 13).
For more than a month now, frontline healthcare workers have been grappling with lost time with family members and disruptions to their personal routines and plans.
Many have to endure working long hours under a plasticky nursing gown, goggles that could fog up, an N95 mask so snugly-fitted that it could cause a headache over prolonged use, a shower cap and gloves.
They also have to deal with the mental strain of having to keep up with constantly changing standard operating protocols and definitions of suspect cases as the Covid-19 situation rapidly evolves.
Dr Ng Wei Xiang, a senior doctor juggling duties between TTSH’s Emergency Department and the NCID, told TODAY that they are at “version 43” of their clinical protocol as of Thursday — just 50 days after the first Covid-19 case was announced here.
In recognition of their invaluable role, along with the sacrifices that come with it, Deputy Prime Minister Heng Swee Keat announced in Parliament on Feb 28 that public officers directly battling the disease will get a special bonus of up to one month, while a one-off Covid-19 grant will be given to 900 PHPCs, including more than 600 GP clinics, which had been activated to deal with the public health crisis.
As Singaporeans adjust to living with Covid-19, TODAY spoke to some 20 frontline workers to get a glimpse of how their lives had been upended by the pandemic.
MITIGATING RISK IN THE FAMILY
In the initial days of the outbreak, when alarming numbers of reported deaths from China dominated the news daily and struck fear in the hearts of many, Dr Leong could sense from chat groups that many of his peers in the GP community were “very stressed out”.
One Sunday in early February, Dr Leong, who doubles up as a leader of a primary care network under the Ministry of Health (MOH), got a call from a fellow GP.
The caller asked Dr Leong to look after his young children should he die from the virus, and to explain to them how he died when they are older.
“It is still early! Why are we talking about dying?” Dr Leong remembered saying in reply.
Dr Philip Koh, 54, a GP with a Healthway Medical branch in Tampines, said a young doctor had also shared with him that for the first time, he had told his father “I love you”, just in case he dies from Covid-19.
While such anxiety has since subsided as more scientific information of the virus emerges, some GPs today, especially those with young kids and elderly parents, still remain adamant about not taking chances in risking the lives of their loved ones.
Among them is Dr Lee, a GP who goes beyond the MOH requirements to wear the full PPE for every single patient he sees.
Inevitably, his outfit had attracted the attention of some of his patients, said the doctor who declined to give his full name.
But the 35-year-old, who practises in an Aljunied clinic and works part-time as a locum, would explain to them that it is his way of protecting his two-year-old daughter who is also looked after by his parents who are entering their 70s.
“When I go to work, the first thing I care about is my daughter and my family. Although I care about my patients, my family comes first… I don’t want to infect them. If an elderly gets it, it becomes bad and can turn into an ICU (Intensive Care Unit) case,” said Dr Lee, whose wife is also a GP.

DEALING WITH PATIENTS WHO ARE NOT UPFRONT
The full PPE is all the more necessary for him, as he had observed a trend of patients making false declarations that they had no respiratory symptoms at the front counter of the clinic, only to “ambush” him by coming clean to him about their runny nose, sore throat or cough in the consultation room.
Typically, a clinic following PHPC guidelines would have triage staff segregating patients who better fit Covid-19 suspect case definition from other patients to minimise any cross-transmission. The process also ensures that the GP could be forewarned to don the PPE before seeing higher-risk patients.
Dr Lee got so irritated with such irresponsible behaviour that he decided to take a tally during a shift on March 5, and found that five out of the 20 patients he saw within a two-hour period were not upfront about their medical condition.
“It beats me why they don’t declare… They lie even when the triage staff warned them twice about the consequences of what might happen to them if they don’t declare,” said Dr Lee.
“I put my life on the line to help, so I am asking the public to be more socially responsible.”
MANPOWER SHORTAGES, FAMILY MEMBERS CHIPPING IN
Dr Clarence Yeo, from Killiney Medical Clinic in the River Valley area, had been working almost daily since February. He believes this would be “useful for the patients”, since MOH had advised that a patient should be reviewed by the same GP if they continued to develop symptoms after consulting one.
The 47-year-old GP who sees an average of 50 to 60 patients daily — about half of them coming in with fever, flu or cough — said he will wait for the number of Covid-19 cases here to dwindle before considering taking leave.
Asked when that might be, he said: “It is very hard to predict. We can’t say the next month, May, or June.”
Regardless, he is ready to put in the hours for as long as the outbreak drags on.
In his second televised address to the nation on the Covid-19 situation on March 12, Prime Minister Lee Hsien Loong said the outbreak “will continue for some time — a year, and maybe longer”.
GPs are not the only ones who are struggling with staffing woes. Manpower shortages and extra shifts are also common at restructured hospitals.
TTSH’s Dr Ng’s most memorable shift took place on Feb 5, the day after MOH announced Singapore’s first four cases of local transmission detected at Yong Thai Hang, a Chinese health products shop at Cavan Road in Lavender.
It happened to be his very first shift at NCID and an unexpected crowd of 300 worried individuals flocked to the screening centre to get checked for Covid-19, after MOH said it would be getting in touch with people who had recent close contact with individuals with travel history to mainland China.
Dr Ng was the only senior doctor rostered with five junior doctors then.
“That was a very, very bad shift, but we survived because people came from all over to help,” said the 33-year-old.
Before he knew it, manpower was diverted from the team manning the Emergency Department. Two consultants, two registrars and a few more doctors arrived to help at short notice.
And not once did he sense anyone having the attitude of “it is not my problem. I am not manning this post”. “They asked if I needed help even before I asked for help,” said Dr Ng.
BEYOND N95-INFLICTED ‘BATTLE SCARS’
Now imagine having to deal with all these work contingencies while running around covered by a humid, overheated “shell” — the full PPE — amid muggy weather this past fortnight.
Indeed, the hospital frontline workers told TODAY it is common now to end their work day drenched in their own perspiration and dehydrated, as they were reluctant to drink more water, just in case they might need to “degown” often for toilet breaks.
Besides getting “battle scars” — facial imprints, pressure sores, abrasions and even blisters on their nose bridge left behind by prolonged N95 use — some frontline workers are also getting pimple outbreaks.

MORALE BOOSTERS
With all the myriad of challenges, work days now seem to be longer for frontline healthcare workers.
The long shifts get more bearable these days, thanks to morale boosters coming in the form of food, presents and “thank you” notes from members of the public — a marked change from before when some healthcare workers donning their uniforms found themselves being ostracised in public.
The nurses and doctors said they are thankful for the chicken rice, nasi lemak, cookies, bubble tea, skin care products and flowers, among other things, that come their way.
But the gifts that take away all their fatigue are usually the extra special ones from their families.
For TTSH’s Dr Ng, that pick-me-up came via a WhatsApp message during a hectic work day, sent to him from his son’s preschool teacher. It was a photo of his five-year-old holding up a drawing paper on which he wrote: “I love you. Thank you for saving Singapore.”






