‘We can’t afford to make any mistake’: Inside a COVID-19 testing lab in Singapore
For three months, Tan Tock Seng Hospital has been running tests 24/7 in the face of several challenges, from trying to ramp up capacity to warding off staff burnout, all while having to keep standards high.

Testing for COVID-19 is “quite tedious” as CNA Insider discovers in an inside look at how it is done.

This audio is generated by an AI tool.
SINGAPORE: For years, since the 2003 outbreak of severe acute respiratory syndrome in Singapore ended, Tan Tock Seng Hospital’s department of laboratory medicine had been planning for another outbreak like it.
The plan was to equip the lab to do 500 tests per day at full capacity, in support of the National Centre for Infectious Diseases (NCID).
But in March, even before Singapore’s daily cases of Coronavirus Disease 2019 (COVID-19) peaked, the Ministry of Health asked the hospital to look into doing 3,000 tests a day, said TTSH head of laboratory medicine, Adjunct Assistant Professor Partha Pratim De.
It has been difficult, however, for the department to go from 500 tests a day to even 800, which is its maximum capacity now “with the amount of staff and equipment that we have”.
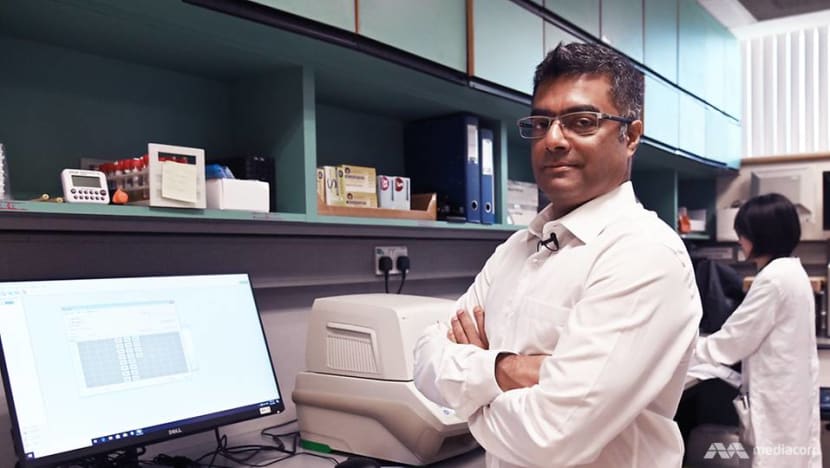
“We’re trying to get staff from here, there and everywhere. We’re trying to get equipment from here, there and everywhere,” he added. “It’s very time-consuming and tiring, but everybody’s working hard in this situation.”
Ramping up testing capabilities is just one of the challenges faced by his lab since the start of the COVID-19 outbreak.
With testing taking place 24/7, staff fatigue is another. And according to lab staff, the process itself is “quite tedious” as CNA Insider discovers in an inside look at how COVID-19 testing is done in TTSH.
“When you’re dealing with hundreds of samples in the middle of the night, every night, it’s very, very difficult,” said Partha De.

IT TAKES AT LEAST THREE HOURS
Singapore’s COVID-19 testing capacity has risen from a daily average of 2,900 tests early last month to more than 8,000. There are now a number of places — from hospitals to public and private labs — where samples are being tested.
At TTSH, the samples can come from nursing homes, some of the polyclinics and the Institute of Mental Health.
But the bulk come from across the road: Each day, porters carry hundreds of swab specimens in cooler boxes from the NCID to TTSH.
Once the samples are in the lab, “every step” taken by the staff becomes “crucial”, said Partha De. And it starts with ensuring that the label for each sample matches the patient in the lab’s information system.

“You get the wrong sample from the wrong patient at this stage, (and) it's a complete disaster,” added the doctor.
The test itself, called the reverse transcription-polymerase chain reaction (RT-PCR) test, is more than 99 per cent accurate in detecting the presence of the novel coronavirus (Sars-CoV-2). But it still requires every stage of the process to be executed properly.
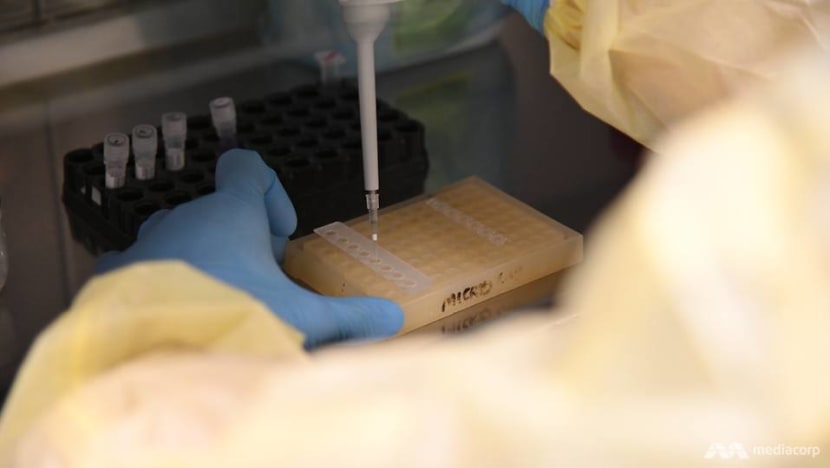
The first stage is the extraction of nucleic acid from the samples. In the room where this is done, the samples are placed in biosafety cabinets that allow only inward airflow to keep any virus particles inside.
Lab staff operating the extractors must also wear personal protective equipment. Their safety tends not to weigh on their minds, however, as the extraction of viral material is a manual process that takes about 90 minutes and requires full concentration.
WATCH: How COVID-19 testing is done in Singapore (7:09)
The material must be extracted into a liquid, which is pipetted into a tube where chemicals known as reagents are used to isolate the COVID-19 viral genome, if it is present.
“Every step of the way, there are protocols to follow,” said medical technologist Nur Ain Lokman from the hospital’s microbiology lab. “Very small volumes of liquids to add ... and such, so one small mistake can affect the result.”
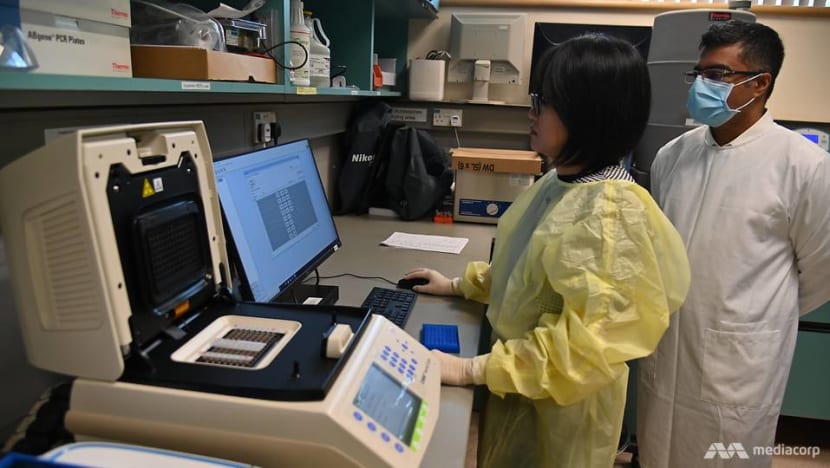
The second stage of the test is the detection phase, which takes another 90 minutes. Here, the extracted samples are mixed with another set of reagents and put in a machine where they are heated up and cooled down.
If the sample has the virus, a reaction would occur that results in the amplification of the viral genome, and thus a positive result is detected.

There are now four machines, each of which can test up to 96 samples. But because the swabs do not arrive all at once, some waiting may be needed and the time needed to report a test result ranges from three to eight hours.
Often, however, there are more samples coming in than the amount that can be tested immediately — a situation that medical technologist Tan Yong Wen described as “mentally taxing’.
“We have to get results fast for the clinicians,” he said. “When it’s a positive (result), it’s faster for them to do contact tracing, and so minimise the spread of the clusters.”
The testing work includes preparing the “master mix” of chemicals to load into the machine, which cannot be contaminated and must be calibrated according to the number of samples.
When the workload is heavy, every detail requires even more focus. “The worst is when it’s 4 a.m. and you still have to concentrate very hard — because we really can’t afford to make any mistakes,” said medical technologist Chua Xian Da.
SMALL TEAM, SUPPLY LIMITATIONS
Ordinarily, the TTSH department of laboratory medicine receives samples mostly from patients to test their blood chemistry, for example, besides testing for communicable diseases like influenza and the Middle East respiratory syndrome, or for viruses such as Zika.
This routine lab work continues, although it has been scaled down from business as usual in tandem with the rest of the hospital’s services to focus on COVID-19.
At the start of the outbreak, TTSH had 13 lab technologists who were trained in the general PCR technique. But they needed training to do a specific PCR test for Sars-CoV-2 after China provided its exact genome sequence.

This diagnostic test, called the Fortitude Kit 2.0 and co-developed by the hospital and the Agency for Science, Technology and Research, was approved on Feb 7.
Soon, the workload at the lab went from a daily average of 250 tests to 370 for a brief period.
“That was roughly the second week of February, around Valentine’s Day, which everybody remembers for the wrong reasons in this hospital,” recalled Partha De.
The 12-hour night shifts were especially tiring.
“At that time, ... the roster was such that (there was) one molecular medical technologist, alone, to process the samples throughout the night,” said Nur Ain. “That required a lot of endurance to sustain yourself, to be able to concentrate throughout.”

The number of night shifts they work has doubled to around four a month, said her colleague Chua. But the staff on duty at night has also doubled, which he reckoned is “better”.
Over the past three months, the team trained to run the RT-PCR test has gradually increased to 22. These include staff within the department, such as junior medical microbiologists, and volunteers with a lab background from other departments.
The training for each of them takes no less than two weeks. “It’s extremely specialised testing,” explained Partha De, who also hired four polytechnic graduates to be rostered only for the night shifts.
Referring to how the RT-PCR is different from rapid serology test kits launched in the market, he pointed out that the latter are blood tests.
“They detect the infection, but after 10 to 14 days of symptoms. That’s too slow,” he said. “The gold standard is still the PCR.”
Increasing testing capacity is not, however, all about having trained manpower. Many countries, including Singapore, are facing a disruption to the supply of extraction reagents required for COVID-19 testing, with shortages mainly in Europe and the United States.
“It’s an international problem. The MOH and the Agency for Logistics Procurement and Supply are now coordinating nationally to distribute extraction equipment and reagent supplies,” said Partha De.
“We’re switching strategy to China, where they have more secure supply lines now that their epidemic problem isn’t as bad. And they’re able to restart factory production for reagents.”
Meanwhile, there has been a reduction in testing of NCID in-patients, who were previously “tested almost every day”, even if they had symptoms.
“Because as soon as they've had two negative swabs, they can be discharged and the bed can be freed up for someone else. But we’ve had to help reduce that,” he added.
“We’re also changing practice based on evidence, so ... we can almost predict when the best time to take a swab is.”
Last month, his department tested a daily average of 420 samples for COVID-19, with the all-time high of 750 tests coming earlier, on March 23.
The lab is now getting more machines and trying out new automations to cut testing times, increase capacity and reduce some of the work done now, such as to manually open each sample tube and add the reagent mixture.
“Otherwise ... we'd begin to see staff fatigue and burnout quite rapidly,” said Partha De.
Read about Singapore’s COVID-19 screening centre, on the front line against the disease.






















