Are we winning in the war against diabetes yet?
Diabetes will be one of three long-term issues which Prime Minister Lee Hsien Loong will focus on during the National Day Rally on Aug 20.

A diabetic patient receives a finger-prick blood test. (File photo: Reuters/Mario Anzuoni)
SINGAPORE: When Dr Bertha Woon sat with her fellow doctors to mull on a topic for Gleneagles Hospital's annual symposium this year, the decision was not hard to make. The focus would be diabetes, which the Government declared war against last year.
In Parliament in April last year, Health Minister Gan Kim Yong declared a war against diabetes, which costs the country more than S$1 billion a year. He announced the formation of a diabetes prevention task force, which he co-chairs with Education Minister for Schools Ng Chee Meng. The task force includes representatives from government agencies, the private sector, patient advocacy and caregiver groups.
In deciding what aspects of the disease to focus on for the symposium that was held in July, Dr Woon, who is the chairperson of the seminar's organising committee, wanted to make sure that it was not confined to just endocrinology, the field that studies diabetes.
She realised one thing: The doctors who came from different specialties all had dealt with patients who were at risk, were pre-diabetic or already had diabetes, but they knew little of one another’s niche area. And that, she realised, is an issue when it comes to the comprehensive treatment of the disease that has caught the attention of the Government.
In fact, Prime Minister Lee Hsien Loong highlighted the fight against diabetes as one of three longer-term issues for Singapore during his National Day message on Aug 8. He will be speaking more on the topic during the National Day Rally this Sunday.
While Type 2 diabetes is a chronic illness characterised by high glucose levels, the number of symptoms and diseases associated with it range from the more commonly known coronary artery disease and obesity to lesser known skin infections.
It may be surprising, but even as a breast surgeon, Dr Woon comes across fungus infections under the breasts or brown patches under the armpits that could indicate diabetes.
“You don’t just target diabetes. A person with pre-diabetes or diabetes may also have things like fatty liver, some marginal kidney problem, or some skin issues that don’t heal. So we look at everything, we don’t just focus on diabetes." It could start with something as minor as a rash, she said.
They don't realise they are diabetic. They may be buying over-the-counter creams and wonder why the rash is spreading. They get a fever and end up in hospital, septic from cellulitis. There's no awareness.
The symposium therefore centred around metabolic syndrome, of which diabetes is a subset. Six speakers from different specialties – an endocrinologist, a renal and internal medicine physician, dermatologist, general surgeon, cardiologist and gastroenterologist – presented during the three-hour symposium.
The symposium was well-received, attended by more than 500 general practitioners and doctors who do not deal with diabetes primarily. It was the best turnout since Dr Woon took over as the annual seminar's chairperson about five years ago, she said.

Based on the most recent figures from the Health Ministry, about 440,000 Singaporeans aged 18 and above had diabetes in 2014. About half of all heart attack patients also had diabetes; two out of five stroke patients had diabetes; and two in three new cases of kidney failure were due to diabetes in 2014, according to figures from the National Registry of Diseases.
There are also more than 1,500 amputations every year – roughly four a day – due to complications arising from diabetes.
HAS THERE BEEN PROGRESS MADE IN THE FIGHT AGAINST DIABETES?
Doctors who spoke to Channel NewsAsia agreed on one thing – that it is too early to tell whether there has been progress in the fight against the disease.
Analyses conducted by the National University of Singapore (NUS) projected that Singapore would have 1 million diabetics by 2050 if nothing is done to combat the onslaught of the disease. Research conducted by the university's Saw Swee Hock School of Public Health, along with the University of Southern California, also estimated that the annual cost of diabetes in the working population would exceed S$2.5 billion by 2050.
These crucial projections on diabetes helped inform the Health Ministry's decision to declare a national "war on diabetes", said Professor Chia Kee Seng, the dean of Saw Swee Hock School.
The diabetes threat in Singapore is a complex problem, he said. “We should avoid oversimplifying the issues and turning to quick and easy solutions for immediate results. The solutions need to be sustainable in order to effectively address systems-level gaps as well as initiate and support long-term individual behavioural and lifestyle changes,” Prof Chia said.
"Success can at times be elusive,” he said, adding that diabetes prevention interventions, similar to measures for curbing tobacco use, tend to take long incubation periods before producing significant results and impact.
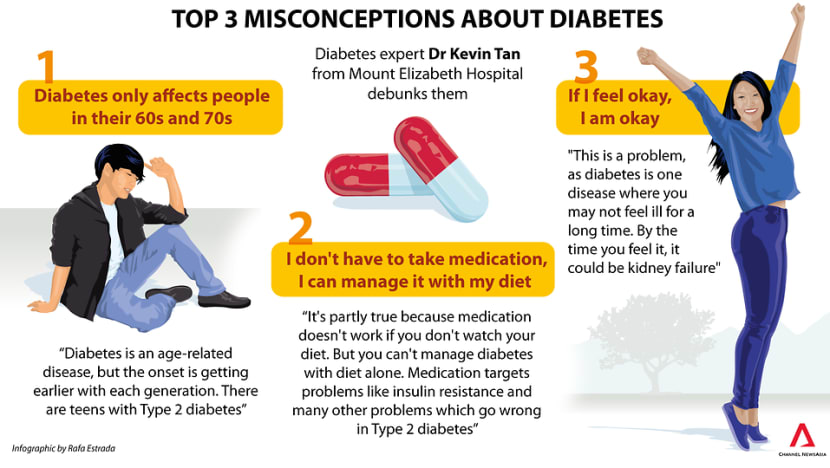
Dr Kevin Tan, consultant diabetologist and endocrinologist at Mount Elizabeth Hospital, echoed the same sentiment. He said it is early days yet, and that it is only after information and awareness “filter to each and every one” through commercials and health programmes that it would be possible to see changes.
The results are not measured in months or even years, it may be a generation or two because we have to change habits.

The slew of initiatives or programmes that were launched as part of the war against diabetes are still in the early stages and these efforts may take several more years before positive results can be seen, said head of SingHealth Duke-NUS Diabetes Centre, Dr Bee Yong Mong.
"We will need to take a mid- to long-term view in the fight against diabetes," he said.
PROGRAMMES TO DRIVE THE MESSAGE HOME
The People’s Association (PA) grassroots organisations have worked with various agencies to reach out to residents, particularly those at higher risk of diabetes such as the elderly, to engage them in programmes and activities so as to help them lead a physically and socially active lifestyle, a spokesman said.
Groups that have been active in disseminating information and increasing awareness on diabetes are the PA Malay Activity Executive Committees Council (MESRA) and the PA Women’s Integrated Network (WIN) Council and the Women’s Executive Committees (WECs).
In September 2016, MESRA spearheaded a six-month nationwide campaign called Let’s Be Healthy - Say No To Diabetes, together with the Malay Activity Executive Committees (MAECs), grassroots and community organisations to fight diabetes in the Malay-Muslim community.
A total of 52 health carnivals and fiestas were organised by the MAECs aimed at raising awareness about diabetes, various chronic diseases and their health risks.
Among the programmes and activities were health screenings, fitness programmes, healthy cooking workshops, health talks and exhibitions, and interactive games.
MESRA chairman Omar Ismail said that while close to 27,000 residents turned up at the events, just a fraction – about 2,700 – underwent medical screenings that were provided free.
“They know that something may be wrong, but they are frightened to confirm it. We don’t give up. We take every opportunity to persuade them to go for the screening,” he said.
He said he observed that Malay-Muslim residents tend to take the disease lightly, so the talks are important.
They don’t understand the dangers of diabetes and the complications it can cause. They don’t have that knowledge.
Recognising that many women are the primary caregivers and they exert strong influence over their family's dietary and healthy habits, the WIN Council and the WECs organised a health carnival in April, and launched cooking classes focused on healthy recipes, with support from the Health Promotion Board (HPB).
To date, 30 healthy cooking classes have been conducted at community clubs islandwide, with another 20 classes to run until December. In addition, about 200 WEC members had attended courses on healthier catering guidelines conducted by HPB.
Separately, the Siglap CC Indian Executive Activity Committees chipped in with a BEAT Diabetes Awareness Day in July, which featured a mass workout session, health screenings, talks and cooking demonstrations.
The SingHealth Regional Health System also runs a diabetes screening programme in an effort to partner community organisations to conduct health screenings for parents, siblings and children of individuals with type 2 diabetes. It also runs a Gestation Diabetes Mellitus Programme. Since January 2016, all expectant mothers at KKH and SGH have been offered screenings for gestational diabetes. A structured protocol has also been implemented for the postpartum follow-up and monitoring of these mothers.
STARTING AWARENESS EARLY
Learning about diabetes in adulthood may prove too late, so the Ministry of Education (MOE) works with students and their parents to encourage active and healthy lifestyles. For example, the Health Ministry and MOE released the NurtureSG Action Plan Report in July, in which one of the key focus areas is promoting physical activity and good nutrition to children and youths.
Physical Education (PE) curriculum time has increased from between one and one-and-a-half hours a week to between two and two-and-a-half hours. These lessons may also include maintaining good eating habits and regular exercise. For example, through a series of PE Journals entitled An Active and Healthy Me, pupils from Primary 1 to 6 levels complete tasks such as recording their food consumption in a week, reading food labels, and planning healthy meals and physical activities with their families.
Under the NurtureSG recommendations, schools also provide more opportunities for physical activity by increasing access to sports equipment and facilities during recess and after school hours.
Efforts have also been made to provide healthier food in canteens. Since January, all mainstream schools have also started implementing the HPB's Healthy Meals in School Programme. Under the programme, set meals provided in school canteens are made from healthier ingredients, prepared by healthier methods, and incorporate food from the four main food groups – whole grains, meat, vegetables and fruits.
Such an early start may be imperative, going by the stark reality of earlier onset. SingHealth Duke-NUS Diabetes Centre's Dr Bee said the centre is seeing more patients who are below the age of 40 compared to a decade ago.
"The youngest patient with Type 2 diabetes on follow up at SGH is 18 years old, and there are patients younger than 18 with Type 2 diabetes on follow-up at the paediatrics unit in KK Women's and Children's Hospital," he said.
RESEARCH EFFORTS AS WORTHY SOLDIERS IN WAR
Initial findings from one of 11 research projects on diabetes at NUS' Saw Swee Hock School of Public Health found that even as Singapore’s overall obesity rate is increasing, the highest increase is among young men, particularly those below 39 years old.
“One likely reason is that they have not adjusted their diets and physical activity levels to correspond to the lifestyle changes that accompany their transitions in life,” said Prof Chia. These transitions include that from full-time national service to working life, and from singlehood to married life and parenthood.
Efforts to combat diabetes must address these lifestyle factors, he said.
Another study that has yet to be published identified five different disease development trajectories and the associated factors. “This can potentially contribute to the development of management plans that are more targeted and customised to the individual,” said Prof Chia.
The school has set aside S$1 million to fund the 11 projects.
Over at Lee Kong Chian School of Medicine at the Nanyang Technological University, metabolic diseases such as diabetes are one of the focus areas in research. The school has also invested in technologies to help understand diabetes and an individual's disposition to developing the condition, a spokesman said.
Professor of metabolic medicine Bernhard Boehm, with postdoctoral research fellow Dr Hou Hanwei, developed a lab-on-a-chip device to better identify diabetes patients with low-level inflammation.
The device has been designed for point-of-care testing, so that treatment can be adjusted in the same doctor's visit rather than in a follow-up appointment. With the additional information, clinicians can better decide the drugs or dosage that are most effective for a patient.
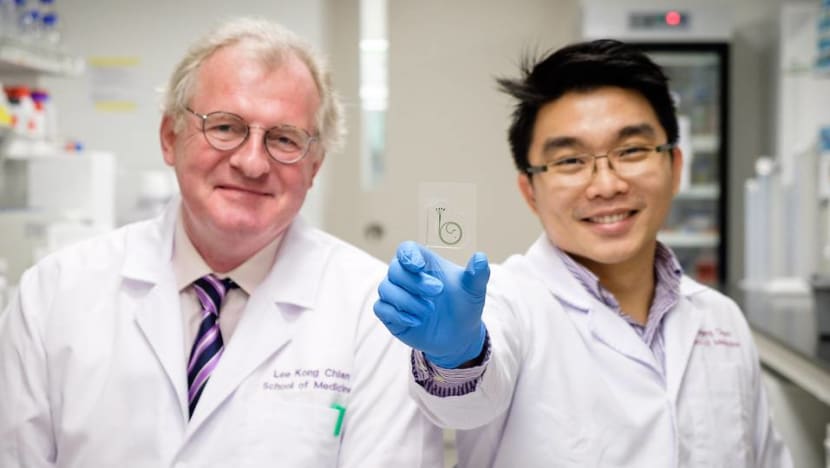
Prof Boehm is also working on novel blood-based signatures of diabetes mellitus, including markers for vascular stress and novel markers that pick up when the insulin-producing cells of the body begin to function abnormally.
“It is well known that the insulin-producing cells of the body, in charge of controlling the blood glucose in a fasting state as well as after a meal, are failing more rapidly in Asians compared with Europeans. Novel blood-based markers could therefore provide a better insight into the pathobiology of this process in Asians,” he said.
PREVENTING AND IMPROVING DIABETES POSSIBLE
It is not inevitable that diabetes will progress, and lead to complications, Dr Woon said. She said doctors shared motivational stories of patients whose conditions improved after they adopted better eating habits, and exercising.
"They then became less reliant on medicines, and didn't have to take strong medicines," she said.
In fact, cutting 5 to 10 per cent of body weight can improve conditions, she said. For those who are pre-diabetic, it can also prevent the onset of the disease.
Technician Mylwahanam Rao experienced this first-hand. The 57-year-old weighed 90kg at his heaviest in 2013. At his annual company medical screening, his doctor warned that his sugar and cholesterol levels were higher than usual. He was also concerned about Mr Rao's family history – two of his diabetic brothers had died of heart attacks in their early fifties.
The screening was a wake-up call for Mr Rao, who had a penchant for murukku and other fried crackers while watching television. He would also eat unhealthy food throughout the day, starting with fried noodles before he got to work. At 10am, he would have another round of fried noodles, before proceeding to have an equally unhealthy lunch. He would have snacks at about 7pm, then a heavy dinner at 10pm just before heading to bed.
He decided he had to make a change so that his health did not deteriorate. In 2014, he cut back on snacks, and started on a healthy diet that included a meal replacement drink, more lean meat, 4L of water and lots of vegetables and fruits. He also walks around his estate for half an hour. Since then, he has lost 8kg.
At following reviews and screenings, his cholesterol and sugar levels have been healthy, he said.

WILL A SUGAR TAX WORK?
The World Health Organisation (WHO) called for all countries to impose a tax on sugary drinks last year, on the back of success through such a system.
The WHO said in a report in November 2016 that a tax of 20 per cent or more in the retail price of sugary drinks results in a proportional drop in their consumption.
Reduced consumption of sugary drinks means lower intake of “free sugars” and calories overall, improved nutrition and fewer people suffering from obesity, diabetes and tooth decay, the report said.
Free sugars refer to ingredients such as glucose or fructose and sucrose added to food and drinks, as well as sugars naturally present in honey, syrups, fruit juices and fruit juice concentrates.
“If governments tax products like sugary drinks, they can reduce suffering and save lives. They can also cut healthcare costs and increase revenues to invest in health services,” the WHO said.
Berkeley, California was the first in the United States to levy a penny-per-ounce tax on soda and other sugary drinks to try to curb consumption and stem the rising tide of diabetes and obesity.
The tax came into effect in March 2015. In a report in the American Journal of Public Health in October last year, residents of two low-income neighbourhoods reported drinking 21 per cent less of all sugar-sweetened beverages and 26 per cent less soda than they had the year before. However, other studies have appeared to show that the effectiveness is decreasing.
Nearby, Mexico has been touted as a better success story. The country, which introduced a 10 per cent levy on sugar-sweetened drinks, has seen a 5.5 per cent drop in sugary-drink purchases in the first year and a 9.7 per cent decline in the second year.
However, not all stories are as sweet. In October 2011, Denmark introduced a tax on food high in saturated fat. A year later, it repealed the “fat tax” and dropped plans for a sugar tax, saying the "fat tax" had encouraged consumers to cross into Germany to shop, unintentionally increased the price of everyday food items and did not change eating habits.
Ireland and the United Kingdom are expected to enact sugar taxes in 2018.
While the Singapore Government has not announced such plans, MPs in Parliament in April last year raised suggestions that included imposing a sugar tax.
Dr Tan from Mount Elizabeth Hospital, who is also vice-president at the Diabetic Society of Singapore, said that currently, healthy food is more expensive in Singapore. Imposing a sugar tax would be beneficial, and that it helps to send a message, he said.
“Taxing unhealthy food can make people veer away if the tax is prohibitive,” he said. However, he cautioned that people who are off sugar may binge on other unhealthy foods, as they feel they are living healthy.
Gleneagles Hospital's Dr Woon said that for the tax to work, there has to be a tangible use for the taxes collected.
She gave an example of an office canteen. “If the tax goes into a fund that is in turn used to buy fruits for staff, they would have a stake in it, and there will be more buy-in."