commentary Commentary
Commentary: Public attitudes of HIV have not moved beyond narratives of fear, prejudice from early years of global epidemic
Singapore’s social acceptance of HIV still lags behind scientific progress, says Mr Rayner Tan and Associate Professor Hsu Li Yang from the National University of Singapore’s Saw Swee Hock School of Public Health.

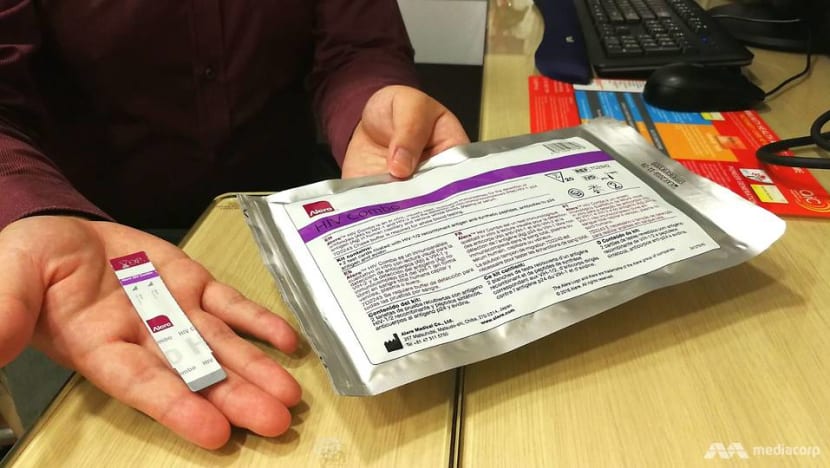
A file photo of blood being drawn during an HIV test. (File photo: AFP)
SINGAPORE: The first diagnosis of a human immunodeficiency virus or HIV infection in Singapore was made in 1985. The incidence of HIV infections has increased every year since then until 2008.
Today, the rate of new infections has stabilised and had even started to decline over the past few years, with just 434 new infections registered in 2017. A total of 7,982 Singapore residents were registered as being HIV-positive as of end-2017, of whom 6,022 remain alive today.
HIV targets a key cell that orchestrates the body’s immune response to a large number of infections and diseases. Left untreated, all infected individuals eventually succumb after a number of years in which their immune systems progressively weaken as more of these cells are destroyed until their body is unable to fight off opportunistic infections and cancers that rarely affect healthy people.
HIV is primarily spread by unprotected sexual intercourse. Other modes including contaminated needles, mother-to-child transmission and blood transfusions are rare, especially in Singapore, due to improvements in needlestick injury protocols, better antenatal care and effective antiretroviral regimens, as well as better screening of blood donors and products.
NO LONGER A DEATH SENTENCE
Marked scientific progress has been made since the start of the global HIV epidemic all those decades ago.
Although a cure or vaccine for HIV remains elusive, when treated, people living with HIV may achieve viral suppression or an undetectable viral load – meaning they do not have a measurable amount of HIV virus in their blood.
Advances in medical science, coupled with a regime of lifetime medication has reduced HIV infection from a death sentence to a chronic disease, with life expectancies close to that of an individual without the HIV virus.
READ: 'It's a death sentence' - HIV myths debunked
More importantly, from a public health standpoint, individuals who achieve viral suppression are at virtually zero risk of spreading HIV to others.
Evidence from three large international observational cohort studies have shown that no transmission of HIV from a sexual partner with an undetectable viral load in nearly 130,000 acts of condom-less penetrative sex.
THE STIGMA REMAINS, EVEN AMONG NURSING AND MEDICAL STUDENTS
However, progress towards social acceptance and the de-stigmatisation of HIV has lagged behind scientific progress in most parts of the world, including Singapore.

Public perceptions and attitudes towards people living with HIV have not moved beyond the narratives of fear and prejudice that marked the early years of the epidemic.
In a 2007 National Behavioural Surveillance Survey, only 54.1 per cent of 1,768 Singaporean survey respondents said they were willing to care for an HIV-infected relative, while only 22.4 per cent were willing to share a meal with an HIV-positive individual.
The results of a survey on the attitudes of 80 nursing and medical students in Singapore towards HIV were highlighted in an editorial in the Annals of the Academy of Medicine of Singapore in 2009.
37.5 per cent of respondents said they would not share a house with a person living with HIV. 34 per cent believed that it was the patient’s fault that he or she had HIV. 20 per cent would not perform surgery on a HIV-positive patient.
These and other studies suggest the stigma surrounding HIV remains prevalent in Singapore, even among professionals who might be called upon to administer care to the people they so stigmatise.
WE NEED TO MOVE BEYOND THIS NARRATIVE OF FEAR AND PREJUDICE
As a hub for healthcare excellence and innovation, Singapore is well-positioned to contribute to the global fight to eradicate HIV by eliminating new transmissions and ensuring all HIV-positive individuals have access to effective treatment.
However, we must tackle this stigma because it has very real implications for HIV transmission and prevention, and may prevent us from achieving the goal of zero new transmissions of HIV in Singapore.
HIV-related stigma is a key barrier to testing for HIV, while the internalisation or anticipation of such stigma among people living with HIV may lead to a late diagnosis of HIV, poor adherence to medication, and poor mental health outcomes.

READ: We still fail to understand that some people are more prone to mental illness, a commentary
These negatively impact HIV prevention because early diagnosis and treatment ensures earlier viral suppression, thus rendering it non-transmissible.
The Infectious Disease Act mandates that all individuals who test positive for HIV at any healthcare provider must be registered with the Ministry of Health within 72 hours of their diagnosis.
However, many fear the repercussions being on the register may have on their career prospects, and the reactions from their friends, colleagues, and family members if they were to find out about their HIV status.
MOH subsequently introduced the anonymous testing scheme in 1991 to encourage HIV testing, and there are a total of 10 designated anonymous test sites today.
READ: Why does Singapore need an HIV registry
In order to receive care and treatment for HIV in Singapore, however, individuals who previously tested positive anonymously will still have their HIV status registered with MOH by their healthcare providers.
The only option to avoid being on the HIV registry while undergoing treatment is to obtain the treatment overseas, a luxury few can afford.
TESTING REMAINS LOW
In spite of the availability of anonymous and affordable testing, voluntary testing rates remains sub-optimal among individuals at risk of acquiring HIV in Singapore.
Only 23 per cent of new HIV infections were detected via voluntary testing in 2017. Yet, only an estimated 72 per cent of Singaporeans who were living with HIV knew about their status in 2015, according to Senior Minister of State for Health Dr Amy Khor who highlighted this in her opening speech at the Singapore AIDS Conference in 2018.
We worry that MOH’s announcement of HIV registry data leak this past week may erode the public’s trust in the integrity and confidentiality of the Singapore’s HIV registry, which in turn may further exacerbate the fear of being registered as an HIV-positive person in Singapore.
This potentially further disincentivises non-anonymous HIV testing locally, and may lead to delayed treatment among those living with HIV, with the consequence of increasing opportunities for the onward transmission of the disease.
But we also see this crisis as an opportunity for Singapore to step up efforts to de-stigmatise HIV and tackle old, hurtful narratives head on.
TACKLE OUR FEARS
The fear of being recorded in Singapore’s HIV registry speaks of a deeper anxiety over one’s own alienation from society as someone living with HIV.
It stems from an overwhelming fear of the impact of disclosure of one’s HIV status to employers, family, friends, and other loved ones. Is it any wonder concealment of one’s HIV-positive status makes more sense to those living with HIV who want to avoid the possibility of discrimination or rejection from those they love?
We must recognise that HIV does not discriminate, but people do. Our response to this incident should be one of compassion and empathy, not only for those whose data were leaked, but also for others living with HIV or the possibility that they might be HIV-positive but are too afraid to find out.
We must recognise that HIV infection is today a chronic disease of public health concern, and not a moral failing.
By doing so, we not only indirectly improve the lives of people living with HIV by destigmatising the disease, but also signal our support for the health of our loved ones and for others in our community.
It is a critical step towards the eradication of HIV in Singapore if we want to achieve that goal in our lifetime.
Rayner Tan is a PhD candidate and researcher on HIV at the Saw Swee Hock School of Public Health, National University of Singapore. Associate Professor Hsu Li Yang heads the Infectious Diseases Programme at the same school.
















