commentary Commentary
Commentary: Inaccurate public understanding of COVID-19 vaccine efficacy has implications for vaccination rates
High vaccination uptake is key to easing COVID-19 restrictions, but a majority of polled respondents misunderstand how much protection vaccines provide, say Clarence Tam, Hannah Clapham and Yung Chee Fu.

A COVID-19 vaccination centre for students on Jun 3, 2021. (Photo: Facebook/Ministry of Education)
SINGAPORE: Eighteen months into the pandemic, we have multiple COVID-19 vaccines available. This is cause for great optimism.
Scientific trials have shown that several have efficacies well above the minimum 50 per cent required by the World Health Organization (WHO). Some, like the mRNA vaccines used in Singapore, have efficacies above 90 per cent.
The amount of information on these vaccines, however, is also a source of confusion. Studies show that, given the choice, people prefer vaccines with a higher vaccine efficacy number and fewer side effects. Media reports interpreting the latest findings from vaccine studies have understandably led the public to compare which vaccines are safer and which offer better protection.
Unfortunately, the scientific community has not communicated clearly what vaccine efficacy means. Therefore, there is misunderstanding about how much protection different vaccines provide and their implications for people deciding whether to get vaccinated.
To get an insight on how the public interprets vaccine efficacy, we polled Facebook users in Singapore to see what they thought vaccine efficacy meant.
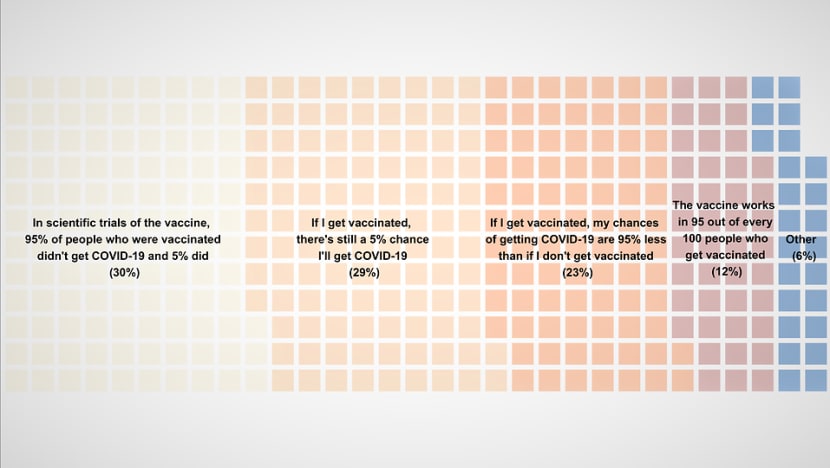
Only a quarter of users identified the accurate interpretation – if vaccine efficacy is 95 per cent, your chances of getting COVID-19 will be 95 per cent lower if you are vaccinated than if you are not.
Instead, most people are under the impression that if you get vaccinated, you still have a 5 per cent chance of getting COVID-19.
This suggests that many people have an inflated sense of their risk of COVID-19 if they get vaccinated, and this could undermine confidence in how much benefit these vaccines provide.
READ: Commentary: Misinformation threatens Singapore’s COVID-19 vaccination programme
This misinterpretation is understandable – what most people want to know is how likely they are to get COVID-19 if they get vaccinated.
But this is not exactly what vaccine efficacy measures. Your chances of getting COVID-19 depend not just on how good the vaccine is, but also on how much virus is circulating in the population and other factors that affect your risk of COVID-19.
These factors include your age, if you have underlying medical conditions, if you work in a high-risk job, how much social interaction you have and your mask-wearing and hand hygiene practices.
Vaccine trials do not generally account for all of these social and lifestyle factors, so they provide limited information about your individual risk of contracting COVID-19.
READ: Commentary: Why many under 45 are hoping vaccination slots open in June
WHAT VACCINE EFFICACY MEANS
We can illustrate the idea of vaccine efficacy with an example from a scientific trial of the Pfizer-BioNTech vaccine, currently used in Singapore.
In that trial, around 36,000 people were randomly split into two groups. Half received two doses of the vaccine, while the other half got two doses of an identical-looking but inactive placebo injection. Everyone was then observed for about six weeks to see who developed COVID-19.
In the 18,000-strong control group who received the placebo injection, there were 169 symptomatic COVID-19 cases over the six weeks. This equates to a risk of getting COVID-19 of about 90 cases for every 10,000 unvaccinated people for this period.
In contrast, in the 18,000 vaccinated individuals, there were only eight symptomatic COVID-19 cases, or about four cases for every 10,000 vaccinated people.
This means that among vaccinated people, the chances of getting symptomatic COVID-19 were about 20 times lower, or 5 per cent of the risk compared to people who got the placebo injection.
READ: Commentary: Why is COVID-19 surging in the world’s most vaccinated country?
Consequently, the vaccine has an efficacy of 95 per cent, because in vaccinated people it reduces the risk of getting symptomatic COVID-19 by 95 per cent compared to unvaccinated people. But it does not mean that 5 per cent of those who got the vaccine went on to get COVID-19.
To date, the risk of getting COVID-19 in Singapore has been very low. Over 2020, before vaccination began, there were about 2,400 community cases in a population of around 5.4 million people living in the community. So for a resident in Singapore, the chances of getting COVID-19 in 2020 were about 1 in 2,250.

Had the Pfizer-BioNTech or Moderna vaccines been available then, getting vaccinated would have reduced this risk by about 20 times, to around one in every 50,000 vaccinated individuals.
Recent increases in community cases mean your risk of getting COVID-19 is currently somewhat higher, but getting vaccinated will still drastically reduce your chances of getting COVID-19.
COMPARING EFFICACIES ACROSS VACCINES CHALLENGING
There has been much interest in which vaccines have better efficacy. Yet, comparing efficacy numbers for different vaccines is not straightforward.
Trials of different vaccines were done in different countries with varying levels of virus transmission, at different time points in the epidemic and with different virus variants circulating.
The trials were also done with different groups of volunteers – some included older adults, while others included mostly younger people who tend to have milder illness. And different trials diagnosed COVID-19 in slightly different ways.
All these influence the estimated efficacy. It is also important to note that headline vaccine efficacy numbers indicate the level of protection against any symptomatic COVID-19 disease.
READ: Commentary: Variants versus vaccines is becoming the new COVID-19 race
For the majority of individuals, COVID-19 is relatively mild, so it is more important to know how well these vaccines protect against severe disease.
The evidence so far is that most of the vaccines available are highly effective for preventing COVID-19 hospitalisation and death, even if some vaccines provide better protection against milder disease.
UNDERSTANDING THE USE OF ALTERNATIVE VACCINES
It is important to interpret vaccine efficacy figures in relation to how much virus transmission is currently happening. The current low levels of transmission put Singapore in an advantageous position.
READ Commentary: Targeted travel restrictions needed but careful not to undermine Changi Airport's connectivity
With rapid scaling up of vaccination, we can drastically reduce the COVID-19 risk in the population and maintain it at a low level even as we ease other social distancing measures.
But for this to work, we need a very high uptake of vaccination in the population.
Recent surveys in March suggest that a third of adults are unwilling or still unsure about whether to get vaccinated. So there is still work to do to communicate the benefits of vaccination, address public concerns and reduce hesitation.

The Singapore Government is also taking other steps to improve the vaccination take-up rates.
They recently announced that the second dose of the Pfizer-BioNTech and Moderna vaccines, usually given within three to four weeks, would be delayed to six to eight weeks. This will allow more people to receive their first dose earlier.
Alternatives to mRNA vaccines will also be made available through the special access route. This will provide vaccination options for people who cannot receive the mRNA vaccines, including those with severe allergies.
READ: More than 30,000 people with history of anaphylaxis will be invited to receive COVID-19 vaccine: Ong Ye Kung
With more options available, people may wonder if it is prudent to mix and match vaccines, for example, because of a belief that taking two different vaccines gives better protection, or because of an unpleasant reaction to the first dose of a mRNA vaccine.
It is not recommended to mix and match vaccines unless medically advised, because we currently do not have any information on how much protection this would provide. Different vaccines are designed and tested using specific dosing schedules and regimens.
Doses of alternative vaccines, such as Sinovac, will be limited and it is important that we reserve these for those who need them for medical reasons.
(Are COVID-19 vaccines still effective against new variants? And could these increase the risk of reinfection? Experts explain why COVID-19 could become a “chronic problem" on CNA's Heart of the Matter podcast.)
QUESTIONS REGARDING VACCINATION TO BE TACKLED
The science of COVID-19 vaccines is indeed evolving constantly as we accumulate more information from large-scale vaccination programmes and the emergence of new variants.
For example, it is too early to know how much protection these vaccines will provide against more recent variants, such as the Delta (B16172) variant currently causing global concern, or how long vaccine protection will last.
But vaccination remains overwhelmingly the best way to reduce your individual risk of COVID-19. It is also currently the only viable way to navigate a safe relaxation of control measures while minimising the risk of large epidemics.
This is not to say that vaccination will drive out the virus completely. As we open up our borders and ease restrictions, we need to accept that the risk of introducing the virus into the community will increase and cases will continue to occur.
Having a large fraction of the population vaccinated will vastly improve our chances of managing these clusters without spiralling epidemics overrunning our healthcare facilities, and without having to implement repeated lockdowns.
Dr Clarence Tam is an Assistant Professor at the Saw Swee Hock School of Public Health under the National University of Singapore.
Dr Hannah Clapham is an assistant professor at the same school.
Dr Yung Chee Fu is a senior infectious disease consultant at KK Women’s and Children’s Hospital and an assistant professor at the Duke-NUS Medical School.


















