Diabetes patients turn to technology and programmes to manage condition independently
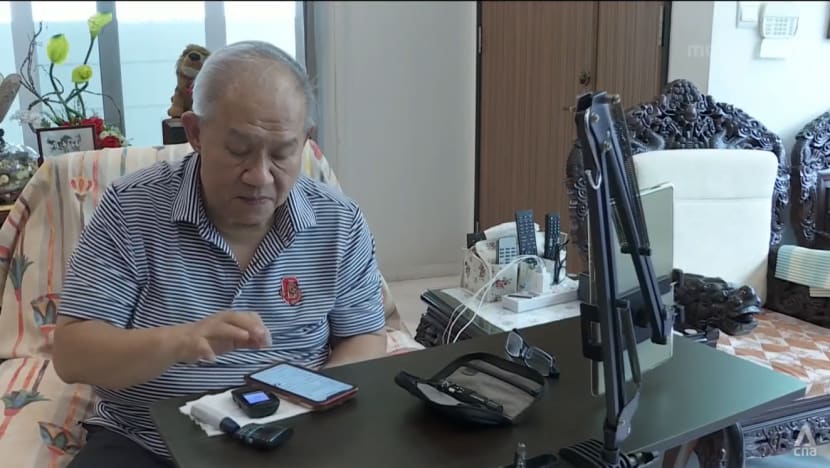
Mr Richard Ng has been living with diabetes for 30 years, but in recent years, he has been using technology to improve his sugar level readings.
SINGAPORE: Mr Richard Ng has been living with diabetes for 30 years, but the turning point for him came five years ago.
His doctor at the polyclinic said things were getting “out of hand” and warned that he may have to start using insulin - often seen as a last resort - to manage his blood sugar levels.
“It will be a phobia for me to go everywhere injecting … so (at) that very moment five years ago, I told him: ‘Okay, I will now focus on my diabetes’,” he told CNA.
The 74-year-old, who was experiencing multiple complications brought on by diabetes, promised that he would adopt better lifestyle habits, and turned to technology to help him.
He now uses a device and app to track his blood sugar levels throughout the day, without him having to manually take down his readings.
The device helps by telling him which foods spike his sugar level, something that will be specific to him and no doctor that can advise him on, he said. He can then avoid these foods.
“The moment I see there's a swing from the regular (reading), then I'm going to scroll back and say what did I eat wrong? What did I eat that has caused my sugar to go up?” he said.
The machine also provides sugar level averages over a week, two weeks and three months, he added.
Mr Ng is among more than 400,000 people here living with diabetes, and this number is projected to rise to 1 million by 2050.
With Singapore having one of the highest prevalence of diabetes cases in Southeast Asia, healthcare providers are turning to such technology and education to improve the way the condition is managed.
EQUIPPING PATIENTS WITH TECHNOLOGY, LITERACY
In the past, doctors may not have been able to get information on their patients’ diabetes control between visits, said Dr Kevin Tan, a consultant in diabetes, endocrinology and internal medicine who runs a clinic in his name.
Technology like mobile apps that help diabetics manage their illness better, and sensors that can continuously track a patient’s sugar levels without the need to prick oneself have clear benefits, he said.
“The technology can help the patient monitor his sugars, manage his condition, correlate his eating habits and his exercise with the sugar data that he's got independent of the doctor in between visits, with the help of feedback to nursing staff,” he said.
“So for people who make use of this technology, for some of them, it has improved their control of diabetes and understanding of the condition."
Besides technology, healthcare providers are also investing in education programmes to better empower patients - in terms of literacy and habits - in a push for more patients to better self-manage their condition outside of the hospital or clinic.
The National Healthcare Group (NHG), for instance, has started a programme to give patients and caregivers a better understanding of diabetes and the long-term care needed.
More than 100 patients have signed up for the programme called Group Education and Empowerment (GEM).
The programme is multidisciplinary, involving doctors, pharmacists, social workers and dieticians.
Physiotherapists, who can teach patients how to exercise safely, are also involved said Dr Yeo Pei Shan, an endocrinology consultant at Tan Tock Seng Hospital.
“Many of us do not dare embark on exercise or don't know how to start and GEM is a starter,” she said.
She said that the programme allows patients to interact with one another and with the team taking care of them.
“We tease out the needs that they have,” she said, adding that patients often do not come forward knowing what they need information on.
BENEFITTING FROM GROUP DISCUSSIONS
Among the patients who have benefitted are Mr Ahmat Pagi and Madam Teo Siew Kee.
"We have to make friends with similar diabetic patients. Then we get more information, how they go through it. The most important is, how we have to take care so that our diabetes does not get worse,” said Mr Ahmat.
For Mdm Teo, who has had diabetes for 35 years, information on handling problems such as low sugar levels in the middle of the night was helpful.
“I feel (like it’s) quite good. We learned a lot. Some people will bring up their problem, they talk a bit, then we listen a bit,” she said, adding that the professionals will guide them.
The initiative is currently available at the Woodlands and Yishun Polyclinics. It will be gradually expanded next year to the other five polyclinics under NHG.



















