IN FOCUS: Men are detecting prostate cancer at a later stage. Why are people shunning a simple blood test?
Fear of cancer, treatment side effects and misconceptions about masculinity may prevent men from prioritising their health, one doctor said.
The number of prostate cancer cases detected at an early stage has declined over time. (Illustration: CNA/Clara Ho)

This audio is generated by an AI tool.
When Mr Chiu Ku Ee went for his annual health screening 12 years ago, his doctor advised him to include a prostate-specific antigen (PSA) blood test as part of his check-up.
He did not think much about it, even when the results showed that his reading was “elevated just above the threshold", the 69-year-old said.
But after being referred for a biopsy when his PSA level rose again, what he had once thought unimaginable came true.
Sometime in 2013, Mr Chiu was diagnosed with prostate cancer.
“I went totally blank and could not comprehend what the doctor was saying anymore,” he said.
“It was a rollercoaster ride after that, both psychologically and emotionally.”
His immediate concerns were how he would continue financially supporting his siblings and elderly mother, and which of the “too many” treatment options he should choose.

After seeing three different doctors who gave him different treatment choices on the best way to manage his stage one diagnosis, Mr Chiu decided to choose active surveillance.
This meant that he would monitor his cancer closely instead of starting treatment.
He waited seven years before he started treatment.
In these seven years, Mr Chiu took it upon himself to gather as much information as he could about prostate cancer.
He spoke to fellow survivors, doctors and read up on information available online, before deciding to undergo stereotactic body radiation therapy in 2021.
He is currently in remission for prostate cancer.
Mr Chiu was one of the lucky ones who managed to get the cancer diagnosed and treated when it was still in the early stages.
While his is a case of picking the right treatment path among the myriad of choices, for many others, the diagnosis of prostate cancer would come far too late and with fewer life-saving options available to them.
MOST COMMON TYPE OF CANCER AMONG MEN
Today, prostate cancer now tops the list as the most common cancer among men in Singapore, data from the Singapore Cancer Registry showed.
From 2018 to 2022, prostate, colorectal and lung cancers were the three most common cancers diagnosed in males, according to the registry’s data. They accounted for 17.4 per cent, 16.2 per cent and 13.4 per cent of cancers diagnosed in males respectively.
The data also showed that prostate cancer’s age-standardised incidence rate, which measures how common new cases of a disease are in a population, had increased from 4 to 38.2 cases per 100,000 men over a five-decade period.
Responding to queries from CNA, a Ministry of Health (MOH) spokesperson said the rise in incidence rate is likely to be partly due to increased screening, as some screen-detected prostate cancers may have remained silent throughout the lifetime of an individual in the absence of screening.
"Prostate cancer is also known to be more common in high-income countries," said the spokesperson.
While prostate cancer rates rose in tandem with the number of screenings, the data also shows that the number of cases detected at an early stage fell more drastically in recent years – a sign that people are only testing for the silent disease when it becomes urgent.
The proportion of prostate cancer patients diagnosed at an early stage fell significantly from 63.5 per cent in the 2003 to 2007 period to 51.6 per cent in the 2013 to 2017 time span.
According to the registry's data on stage distribution of prostate cancer from 2018 to 2022, 15 per cent of prostate cancer cases were discovered in stage one, 29.3 per cent in stage two, 25.5 per cent in stage three and 30.2 per cent in stage four.
These trends are concerning, experts said.
Despite large advances in cancer-related medical technology and the greater availability of prostate cancer screening today, fewer men are catching the disease early.
Stigma and embarrassment about discussing men’s health issues, including prostate cancer, could be why men are reticent about going for tests or talking about their symptoms, said Dr Jeffrey Tuan, a senior consultant of radiation oncology at the National Cancer Centre Singapore and a committee member of Singapore Cancer Society.
"Fear of cancer, treatment side effects, and misconceptions about masculinity may prevent men from prioritising their health," he added.
To uncover the reasons why early detection remains a challenge, CNA spoke to 60 men aged 50 and above to find out their awareness, attitudes and experiences with prostate cancer screening.
Less than half, or 25 respondents out of the 60, have not been for a prostate cancer screening, even though 45 respondents said they go for a health screening at least once every two years.
SCREENING COST, LOW AWARENESS
While some avoided going for tests due to fear or a lack of symptoms, others pointed to the cost of screening.
Prostate cancer screening is currently not a subsidised screening under the national health screening programme, known as Healthier SG Screening.
MOH said it takes reference from the Screening Test Review Committee’s (STRC) recommendations for screening.
"STRC recommends that screening for prostate cancer with the PSA be done on an individual level for those who have a high risk of getting prostate cancer."
The ministry also advises individuals to discuss their risk profile with their doctor and whether prostate cancer screening is appropriate for their individual circumstances before proceeding.
"As such, prostate cancer screening is not included in Healthier SG Screening, and MOH does not track its screening rate," the spokesperson added.
Screening for other types of cancers - colorectal, cervical and breast - as well as cardiovascular diseases, is part of the programme.
"MOH continually encourages Singapore Citizens to enrol with Healthier SG and go for regular screenings and follow-ups. With early detection and appropriate intervention, we can prevent or delay the onset of various conditions and diseases," the ministry's spokesperson said.
CNA also found that knowledge of prostate cancer was low.
Of the 60 respondents, 31 said they had little to no knowledge on prostate cancer, while 32 of them never knew prostate cancer screening existed or had very limited knowledge about it.
Dr Terrence Lim, a senior consultant urologist at Assure Urology, said that while public awareness is “generally good”, that does not necessarily translate to men taking action.
“A lot of times, urinary symptoms are common in older men and many of their friends have that. So they attribute it to ageing,” he said, adding that men are generally less health conscious than women and may not see the need to go for regular screenings.
Assoc Prof Chong Yew Lam, a senior consultant at the department of urology at Tan Tock Seng Hospital, said awareness of prostate cancer in the country is “slightly lower” compared to breast and colorectal cancer, for which screenings are relatively established.
However, as patients become more informed and increasingly turn to online tools for guidance, he has observed that in general, men are taking greater ownership of their health and are more willing to discuss complications and quality of life.
“They want to take more ownership, but still want a trusted peer nearby to bounce off ideas and that has helped the dynamics and decision making for many of them,” he said.

Prof Chong further said that many men may not see the need to go for screening until they start experiencing symptoms. But with prostate cancer, symptoms can sometimes only start appearing in the later stages.
In fact, some patients with stage four prostate cancer may not have any symptoms and might not even realise they have the disease.
“Symptoms themselves are not a very reliable sign of whether a person has or does not have prostate cancer because it overlaps with a lot of other symptoms a patient may have associated with ageing as a healthy male,” Prof Chong added.
An enlarged prostate and urinary changes that can occur in healthy men often “overlap significantly” with the symptoms experienced by patients who have prostate cancer.“
"So it is very hard to use symptoms alone as a singular screening tool.”
Because of the nature of the disease, it is tricky to carry out prostate cancer screening at a large scale.
On this point, Dr Tuan noted that there is an ongoing discussion among the medical community about whether population-wide screening should be adopted.
Said Dr Tuan: "The overall benefits of mass PSA screening are still debated due to over-diagnosis and potential harm from unnecessary interventions."
At the same time, "significant" misconceptions and informational gaps about prostate cancer still persist among men and their families, he said.
"Many men still lack understanding about the disease, its risks, and the importance of early detection," he said.
"Prostate cancer often receives less public, and media attention compared to other major cancers, and this may contribute to delays in seeking medical opinion or screening."
WHAT THE SCREENING PROCESS ENTAILS
With that, Prof Chong is urging men above 50 to go for regular prostate screenings, reiterating that early detection is always better than treatment at a later stage.
This is especially important as the disease might run in the family, he added.
If a patient is diagnosed with prostate cancer and shares that his father or brother also had the disease, Prof Chong would advise the patient's sons to get screened earlier.
"Maybe at 45 years old, rather than 50 or 55," he said.
A patient who is being screened for prostate cancer will first go through a PSA blood test.
When the PSA level is higher than four, a patient is at an increased risk of having prostate cancer.
“In general, someone with a PSA of between four to 10 has a 30 per cent chance of having prostate cancer,” said Assure Urology’s Dr Lim.
But having said that, a normal PSA of below four does still give a patient a 10 to 15 per cent chance of having the disease, he further explained.
Tan Tock Seng Hospital’s Prof Chong echoed this statement, saying that “PSA alone is an imperfect biomarker” and there are cases where patients do not have prostate cancer even if they’re PSA level is above four.
Patients who are suspected to have prostate cancer would then be sent for magnetic resonance imaging (MRI), where they would be given a more accurate picture of their risk of prostate cancer.
“From this, we can then decide whether patients should be triaged to get a biopsy or even avoid a biopsy. If you use PSA alone, you will do a lot of excessive and unnecessary biopsies,” said Prof Daniel Yong, head and senior consultant at the department of urology at Tan Tock Seng Hospital.
“The MRI scan can help us pick up clinically significant prostate cancer that might need treatment, and that’s where we will target the lesions for biopsy,” he added.

Once the biopsy is done and prostate cancer has been proven to be present, doctors will group them based on the Gleason grade group to provide a more accurate prediction of how aggressive the prostate cancer is.
“So we classify it like domestic cats versus wild cats,” said Prof Chong, adding that he phrases low-risk prostate cancer to his patients as “almost good news”.
“You have prostate cancer but it is not aggressive and you can live with it. And we explain to the patients how we’re going to help them live with it by monitoring their condition over the next few years,” he said.
This would include PSA blood tests, and sometimes more MRI scans and future prostate biopsies.
The cancer is also generally categorised as either localised, where it has not spread beyond the prostate, or advanced, where it has spread to other parts of the body.
In advanced cases, the cancer often spreads to the bones, weakening them and making patients more prone to fractures.
For patients who have higher risks, the various types of treatments will be discussed.
“Some of the common questions are what does it mean for them, how widespread the disease is, and what their lifespan is going to be,” Prof Chong said.
Given the anxiety that often comes with a new diagnosis, Prof Chong typically discusses treatment options during the patient’s next visit, after they’ve had some time to come to terms with the news.
“They’re already overwhelmed with the diagnosis, so it’s very important to have a second visit to talk through it, hear their concerns and how they want to be treated,” he said.
Wider range of treatment options, including use of robots
It is not the end of the road when the diagnosis comes back with a positive for prostate cancer, thanks to modern medicine and robotic surgery methods.
The two most common types of treatments are radiotherapy and surgery.
For a patient whose prostate cancer is still localised, doctors would often recommend radiotherapy as it is a “less invasive” treatment option.
Mr Chiu, who sought treatment seven years after his diagnosis, chose stereotactic body radiation therapy, where he just had to go through over less than two weeks.
In cases where there is high or immediate risk, surgery is often recommended where the whole prostate would be removed, but radiotherapy can be done too, said Assure Urology’s Dr Lim.
“Each treatment option has its own pros and cons. So far there’s no head to head study to compare the two options, but both are feasible options that need to be tailored according to the patient’s lifestyle,” he said.
Open surgery - where doctors make an incision from the belly button down to near the root of the penis - is no longer a common approach.
“It has been shown that with open surgery, blood loss is much more and the patients take longer time to heal with longer hospitalisation stays,” Dr Lim said.
Advances in surgical techniques, such as keyhole procedures, have thus significantly reduced recovery times in recent years.
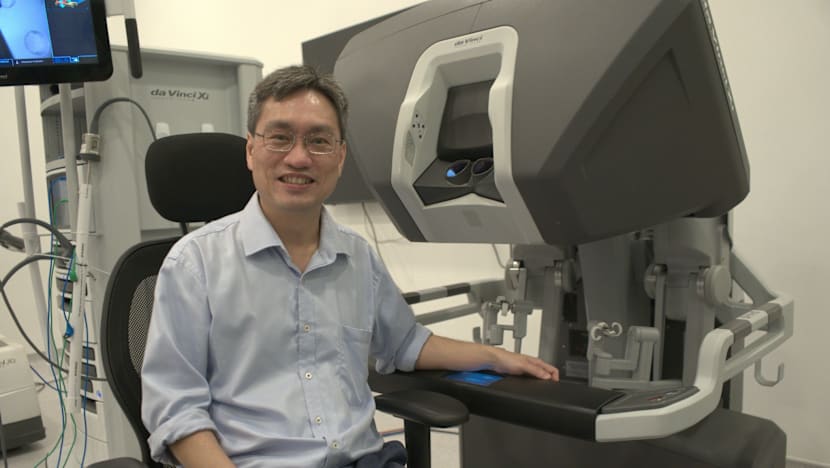
There are two types of keyhole procedures - a conventional laparoscopic surgery and a robotic urologic surgery. Instruments are inserted via a keyhole-sized insertion of about 1cm or less.
Doctors have been increasingly steering towards robotic urologic surgery, as it offers greater precision, improved control, and better visualisation during the procedure.
“Robotic surgery allows for 3D vision, so you do have that perception,” Dr Lim said. “And the magnification of the robot can go up to 10 times, so you can see and operate better.”
Robotic surgery also gives doctors “the degree of freedom of the instrument,” Dr Lim explained. “So it’s like having a wrist that can turn up, down, left and right.”
When trying to explain the differences between both types of keyhole surgery to his patients, Dr Lim would tell them that laparoscopic surgery is like trying to hold a needle with a chopstick to stitch, but robotic urologic surgery will be just like holding a needle in your hand.
“And because we can see better, we can stitch better, the function outcome will definitely be better. And there is definitely less blood loss.”
In open surgery, patients can lose as much as two to three litres of blood. Whereas with robotic urologic surgery, blood loss is usually no more than 200 to 300 cubic centimetres.
For patients who are afraid of a robot doing surgery, Dr Lim often assures them that the machine is just an "extension of the surgeon’s hands.”
“So to me, the robot is a surgical tool rather than an actual robot itself.”
Over at Tan Tock Seng Hospital, 99 per cent of prostate cancer surgeries are done by robotic urologic surgery.
“We still do a couple of open prostate surgeries only in exceptional situations,” Dr Chong said.
In recent years, progress has been made in prostate cancer therapy, said National Cancer Centre Singapore's Dr Tuan.
"The treatment can be carried out on an outpatient basis because the medication is usually taken orally."
"In addition, the side effect profile has also improved significantly. The disease can now be treated efficiently without compromising the quality of life of the patient," he said.
According to data from the national cancer registry, prostate cancer has the highest survival rate compared against other common cancers, with 97.9 per cent and 89.2 per cent of patients surviving at the one-year and five-year mark after they were first diagnosed with it.
THE ROLLERCOASTER RIDE TO BATTLE CANCER
For Mr Chiu, life quickly returned to normal after he completed treatment. He does not experience any side effects from radiotherapy.
But this was not the case for 67-year-old Mr Eddie Low.
When Mr Low was first diagnosed with stage one lung cancer and stage two liver cancer in 2017, it seemed hard to believe that he would be diagnosed with a third type of cancer.
But a PSA blood test, followed by a biopsy, confirmed that he was in the early stages of prostate cancer.
Mr Low was unable to start treatment immediately, as he was still undergoing chemotherapy for lung and liver cancer.
“It’s been a rollercoaster ride, battling with one cancer after another,” he said, adding that this was a challenge for his wife as well.
“I’m already going bonkers, so I can’t imagine what’s on her mind,” he said.
By the end 2018, he too had started on stereotactic body radiation therapy as surgery was not an option for him due to the other two types of cancer he was battling with.
He went through five sessions over six weeks and felt that the process was “quite smooth”.
Although he did not feel any side effects once his treatment concluded, he suffered from radiation cystitis - an inflammation of the urinary bladder - five years after in 2025.

Mr Low described it as a “traumatic experience” as he had to receive treatment for three months to stop the bleeding and is unable to travel until his condition stabilises.
“If my bladder bleeds, it can lead to blood clots and I will not be able to urinate. And I'll be in pain and have to get treated,” he said.
Incontinence - the inability to control urination - and impotence, or the inability to achieve or maintain an erection, are the two main side effects that doctors say can significantly affect quality of life.
“Although in surgery there’s an option of a nerve sparing prostatectomy that is supposed to help you regain the erectile function, the truth is that erectile function will still take a negative hit,” said Tan Tock Seng Hospital’s Prof Yong.
As for incontinence, Prof Yong said how long the person goes through it can vary, but 85 to 90 per cent of patients regain urinary control by the one-year mark.
“But for the remaining 10 per cent of patients, it means a loss of ability to control urine when changing positions, coughing or sneezing within one year,” he said.
On top of receiving “extensive counselling” from doctors who will tell them what to expect during the recovery process, specialised nurses will also teach patients pelvic floor exercises that can help improve their continence rates after surgery.
This can often help patients regain more than 90 per cent continence if done regularly, Prof Yong said.
“In fact, one of the main reasons why some are incontinent even at the one-year mark is due to non-compliance with the pelvic floor exercises,” he said, adding that older men may take a longer time to regain control.
SUPPORT FROM FELLOW SURVIVORS
Yet, support from doctors and nurses can only go so far.
Nothing helps more than speaking to someone who has walked the same path, patients who have undergone cancer treatment told CNA.
During the seven years where Mr Chiu was on active surveillance, he joined Tan Tock Seng Hospital’s prostate cancer support group - the Walnut Avengers.
“Members are very experienced and knowledgeable about what’s going on and they are so open about talking about anything and everything,” he said. “Even family members cannot relate to you as much because they don’t have it.”
Sessions with the support group often included them sharing their lived experiences, outdoor exercises and talks by doctors.
“When other members start asking questions, you learn more and also participate in asking questions. So it really helps to connect the dots.”
“Sometimes we don’t know what to ask the doctor during consultations, but these sessions help you tap on each other to ask anything.”
But Mr Chiu’s favourite part of these meet-ups would be the cup of coffee they would get after together.
“It’s like a brotherhood,” he said.

Though Mr Chiu started off as just a participant 12 years ago, he is now a volunteer that helps newer members navigate their prostate cancer journey.
“They have many worries and speaking to someone who has been through it helps them see the bigger picture,” he said.
Despite still grappling with the side effects from his treatment, Mr Low too has found strength and resilience from his family, faith and support group.
Part of Singapore Cancer Society’s Walnut Warriors, Mr Low said the support group has connected him with older survivours who have dealt with similar side effects.
“They have a couple of years ahead of me and can willingly share when I ask them specific questions about treatment and experiences,” he said.
In return, Mr Low also shares his own personal stories to new members about how he has been living fully despite his side effects.
“I can only give them my advice. I tell them everyone is different and you must look at your situation and what works best. I give them the confidence and hope that cancer is something that can be dealt with.”
“I’m there not to tell them what to do, but to be there for them if they have any questions,” he said.
Mr Low also suggested that awareness efforts seen in breast and colorectal cancer should also be extended to prostate cancer.
“It’s very common to hear of men being diagnosed with prostate cancer,” he said. “A simple blood test can serve as an early guide.”
His advice to men is an easy one.
“Don’t be fearful, take it one step at a time. Early detection makes treatment much easier, and it can save your life.”
















