NTU researchers develop drug-free treatment to kill cancer cells
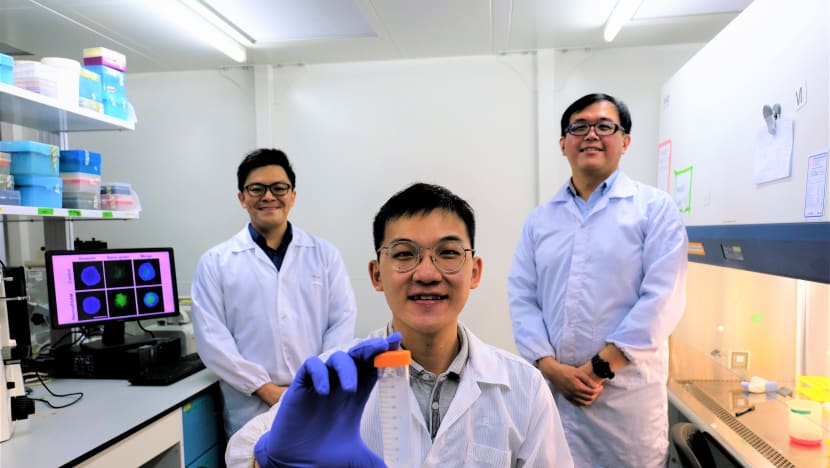
From left: Members of the NTU research team include assistant professor Dalton Tay from the School of Materials Science and Engineering, research associate Kenny Wu and associate professor Tan Nguan Soon from the Lee Kong Chian School of Medicine.
- The new method involves coating silica nanoparticles with an amino acid to trick cancer cells into accepting them
- The cancer cells then self-destruct after accepting the particles
- The nanoparticles killed about 80 per cent of breast, skin and gastric cancer cells during laboratory tests
- Human trials have not been done and it will take about a decade for this method to be adopted by hospitals
SINGAPORE — Researchers from Nanyang Technological University (NTU) have developed a treatment for cancer that does not involve drugs.
The treatment, which is still in the early stages of being tested, involves coating a silica nanoparticle with an amino acid called L- phenylalanine to trick cancer cells into accepting it.
Once the coated particle, named “Nano-pPAAM” by the researchers, enters the cancer cell, it stimulates the production of reactive oxygen species which cause cancer cells to self-destruct.
Assistant Professor Dalton Tay from NTU’s School of Materials Science and Engineering, who led the study, described this method as a “Trojan horse” approach.
“We know that cancer cells have an addiction to amino acids because they need to fuel their growth. By coating our particles with L- phenylalanine, we make them think this is an amino acid that they have to take in order for them to grow… but what we are delivering into the cell is a particle that can kill it,” explained Asst Prof Tay during a virtual briefing to the media on Wednesday (Sept 23).
Currently nanoparticles, which refer to ultrafine particles, are used in chemotherapy for cancer patients.
These particles are usually loaded with drugs and delivered to cancer cells through various means such as direct injection into the tumour or through the bloodstream.
The use of nanoparticles in this way has a number of downsides, said Asst Prof Tay.
These include:
Cancer-killing drugs being chemically or physically incompatible with the nanoparticle material.
Cancer cells becoming resistant to the drug
Non-cancer cells getting destroyed in the treatment process given the toxic nature of the drugs
While there are existing forms of treatment for cancer which do not require the nanoparticle to carry drugs to the cell, such as photodynamic therapy, these treatments require external stimuli in the form of light or heat to stimulate the nanoparticles to destroy the cancer cells, said Asst Prof Tay.
His team’s method is the one of the first few treatments that do not require external stimuli and drugs, he said.
The silica nanoparticle is also not toxic and unlikely to kill non-cancer cells, said Asst Prof Tay, adding that the US Food and Drug Administration has approved its use in food additives.
As a new method, cancer cells are also less likely to be resistant to it although whether cells may develop resistance in the long-run is something the team has yet to study, he said.
Results from laboratory tests have been promising.
The team’s nanoparticle, which is 30 nanometres in diameter, killed about 80 per cent of breast, skin and gastric cancer cells in mice — comparable to conventional chemotherapeutic drugs like Cisplatin.
However, further tests, including human trials, are needed before the method can be approved for use in hospitals and this could take about 10 years, said Asst Prof Tay.
The team is currently applying for a patent for the nanoparticle and is also on the lookout for industry partners to develop it with.
Providing an independent view, Associate Professor Tan Ern Yu, a breast cancer specialist at Tan Tock Seng Hospital, said in a press release: “This novel approach could hold much promise for cancer cells that have failed to respond to conventional treatment like chemotherapy."
Assoc Prof Tan added that as cancer cells have not yet adapted to this new approach, they are less likely to be resistant to this compared to other currently available treatments.












