Commentary: Resolving conflict over ‘vaccinated blood’
How should hospitals respond to patients who refuse blood transfusions or medical treatments due to unfounded COVID-19 beliefs? NUS Medicine’s Professor Julian Savulescu and Dominic Wilkinson from the University of Oxford weigh in.

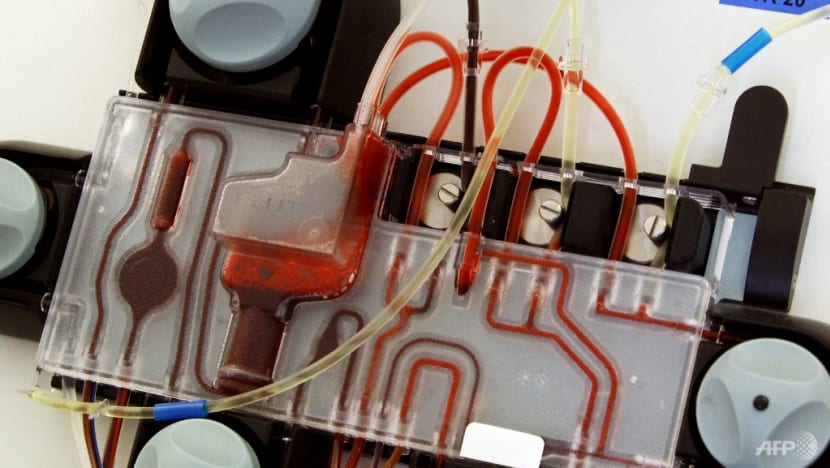
File photo of a doctor collecting blood from a patient. (Photo: AFP/Ana Arevalo)
SINGAPORE: In a recent high profile case, a New Zealand baby, Baby W, was placed under temporary guardianship by the courts after their parents refused blood transfusions from donors vaccinated against COVID-19.
The six-month-old baby needed urgent life-saving heart surgery that would have been impossible without donated blood. The parents’ objection was based on fears that spike proteins from the vaccine would enter and harm their baby.
While rare, this is not a unique case: In Canada, an obstetrician in October tweeted that a patient had indicated she would decline blood from donors vaccinated against COVID-19.
The US has also encountered patients who have refused to consent to transfusions unless they could be assured the blood was from unvaccinated donors, according to a February paper in the British Journal of Haematology.
In Singapore, there have not been any reported cases of patients refusing blood transfusions from vaccinated donors. However, given that nearly 92 per cent of Singapore’s population have received at least one dose of the vaccine, most of the country’s blood supply would be from donors who have been vaccinated. There are a small number of people who have strong views about vaccination, and it is possible that similar situations would arise.
CAN PARENTS REFUSE SURGERY OR TRANSFUSION?
In the case of Baby W, was the New Zealand court right to intervene? How should authorities and hospitals respond to such cases?
Parents are usually closely involved in decisions about medical treatment for their children, but there are limits. Most societies don’t think that parents should be allowed to make decisions that would risk serious harm to their children. For example, parents cannot refuse life-saving treatment.
W’s parents wanted to treat their baby: They agreed with doctors about the surgery and recognised its urgency. They just didn’t want blood from a particular source. But that doesn’t mean they should have been allowed to choose: There are other factors that need to be considered.

ARE THE PARENTS’ CONCERNS JUSTIFIED?
W’s parents’ concerns have been attributed to “misinformation”.
The parents’ concern about the “spike protein” in the vaccine has no scientific basis. There is no evidence that the protein generated by the vaccine is harmful. In any case, it is present in “vanishingly small quantities” initially and not at all after two weeks. Many countries, including Singapore, already have rules that restrict donations for a period after vaccination.
However, even if it is clear that parents are mistaken, it doesn’t automatically follow from this alone that they should be overruled. Although unnecessary, it wouldn’t be harmful to Baby W to receive blood from an unvaccinated donor.
RELIGIOUS ACCOMMODATION AND JUSTICE
It is an important principle of medical ethics that doctors should pay attention to the views and values of patients. They should do that even if the doctor thinks that the patient is mistaken or that their views are irrational.
One common source of disagreement is conflicting religious values. For example, an atheist doctor should try to respect and accommodate a religious patient’s requests for treatment that meets the requirements of their spiritual teaching.
But it also includes non-religious values – for example patients who are vegan or concerned about the climate. Or patients may have particular medical concerns. Doctors should potentially try to accommodate those requests, even if they do not share the concerns.
However, the patient’s values are not decisive. There is one good reason to deny such requests - distributive justice.
Distributive justice is the principle of allocating limited resources fairly. Health resources constitute a limited pie, and everyone is only entitled to his or her fair share.
First, patients do not have the right to demand interventions that are not possible. For example, at present there is no way to identify blood that would be acceptable to Baby W’s parents, certainly not within the time that the infant needed treatment.
A second reason is more important: It would potentially be costly and resource-intensive to implement. Meeting the logistical challenges of identifying blood that would be acceptable to Baby W’s parents (or other recipients) would divert limited resources away from other patients.
A third concern is the security of the blood supply. Allowing parents or patients to pick and choose who they are happy to receive blood from would set a dangerous precedent.
Blood services carefully screen donors to avoid blood products that might present a risk to recipients. If patients are allowed to choose their own preferences, without scientific basis, it might permit some individuals to choose based on discriminatory beliefs. It may undermine the altruism and solidarity upon which the blood donation system is based.
COMPROMISE? DIRECTED DONATION
One option that might allow Baby W’s parents’ views to be respected without requiring major changes to the usual process of blood donation would be through something called “directed donation”.
This is the term used for someone donating blood directly to a specific individual. In this case, Baby W’s family members or friends could have donated blood for the surgery.
But directed donation is not a simple solution. It is associated with slightly higher medical risks for the recipient (for example of infection, of developing antibodies, and of a rare problem called “graft versus host disease”). These risks are relatively small, so it is not clear that they alone would rule out directed donation.
Second, and more importantly, it is not clear that it would be practical in a case like Baby W’s. Directed donation requires extra time to collect and screen the donated blood.
For major heart bypass surgery, the surgery typically requires multiple units of blood products of different types. It is not clear it would be feasible to collect enough of the right kind of blood for the operation in time for it to take place. This would also likely require significant additional time and resources to undertake the collection and screening.
Finally, this may appear to be offering implicit support for a view that has been harmful to society.
Misinformation about vaccines in general and the COVID-19 vaccine in particular has caused and continues to cause preventable serious illness and death on a huge scale.
Individual doctors, or health systems may choose not to accommodate vaccine sceptics, in case this provides tacit support for such views.
UNSUPPORTED BELIEFS SHOULD NOT BE SUPPORTED IN LIFE-SAVING SITUATIONS
Cases like that of Baby W are rare. However, they raise important questions about how much health systems can or should accommodate patients and parents who reject certain medical treatments.
If we allow parents to decline COVID-19 vaccination for their children, it may seem paradoxical that they are not allowed to refuse a blood transfusion from vaccinated donors. However, the consequence of refusing blood transfusion for a seriously ill child is much greater than refusing vaccination in a healthy child.
If a parent’s unsupported beliefs make life-saving surgery impractical, they should not be accommodated.
Professor Julian Savulescu is Director, Centre for Biomedical Ethics at the Yong Loo Lin School of Medicine, National University of Singapore. Dominic Wilkinson is the Head of Medical Ethics at the Oxford Uehiro Centre for Practical Ethics at the University of Oxford.
























